The Veterans Affairs Patient Safety Center of Inquiry—Suicide Prevention Collaborative: Creating Novel Approaches to Suicide Prevention Among Veterans Receiving Community Services
Background: While the US Department of Veterans Affairs has made significant strides to prevent veteran suicide, efforts have largely targeted veterans actively engaged in and eligible for Veterans Health Administration (VHA) care, which is consistent with the VHA mission. The majority of veterans are not enrolled in VHA care, and many are ineligible for services. Veterans not connected to VHA have experienced an increase in suicides in recent years.
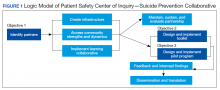
Observations: Since 2018, VHA National Center for Patient Safety has funded the Patient Safety Center of Inquiry-Suicide Prevention Collaborative (PSCI-SPC), which has worked to develop, implement, and evaluate practical solutions aimed at curbing the rising suicide rate among veterans not receiving VHA care. PSCI-SPC has 3 guiding objectives: (1) Develop and test a collaborative, organizational structure to connect VHA and community organizations, such as national, local, public, private, nonprofit, and academic partners who provide high-quality and timely health care; (2) Build and test a learning collaborative to facilitate sharing of VHA suicide prevention best practices with community partners to increase availability, consistency, and quality of mental health services for all veterans; and (3) Implement, test, and refine a novel program to provide affordable suicide prevention interventions to veterans with mental health needs, regardless of their use of, or eligibility for, VHA services. This paper details the current progress for this demonstration project. As these objectives are met, PSCI-SPC will create and disseminate products to support broad implementation of these practices to other VA medical centers and the communities they are embedded in.
Conclusions: PSCI-SPC seeks to fill an important gap in veteran health care by serving as a national clinical innovation and dissemination center for best practices in suicide prevention for veterans who receive care in their communities.
Program Overview
VHA Patient Safety Center of Inquiry-Suicide Prevention Collaborative (PSCI-SPC), funded by the VHA National Center for Patient Safety, aims to help fill the gap in community-based suicide prevention for veterans. PSCI-SPC is located within the VHA Rocky Mountain Mental Illness Research, Education, and Clinical Center in Aurora, Colorado. The overarching mission of PSCI-SPC is to develop, implement, and evaluate practical solutions to reduce suicide among veterans not receiving VHA care. PSCI-SPC serves as a national clinical innovation and dissemination center for best practices in suicide prevention for organizations that serve veterans who receive care in the community. PSCI-SPC creates products to support dissemination of these practices to other VAMCs and works to ensure these programs are sustainable. PSCI-SPC focuses on 3 primary objectives. All PSCI-SPC projects are currently underway.
Objective 1: Growing a Community Learning Collaborative
Acknowledging that nearly two-thirds of veterans who die by suicide do not use VHA services, PSCI-SPC aims to reduce suicide among all veterans by expanding the reach of best practices for suicide prevention to veterans who receive myriad services in the community.27 Community organizations are defined here as organizations that may in some way serve, interact with, or work with veterans, and/or employ veterans. Examples include non-VHA health care systems, public services such as police and fire departments, nonprofit organizations, mental health clinics, and veterans’ courts. As veterans increasingly seek health care and other services within their communities, the success of suicide prevention will be influenced by the capability of non-VHA public and private organizations. Objective 1, therefore, seeks to develop a VHA-community collaborative that can be leveraged to improve systems of suicide prevention.
Current programs in the VHA have focused on implementation of suicide prevention awareness and prevention education campaigns instead of grassroots partnerships that are intended to be sustainable. Additionally, these programs typically lack the capacity and systems to sustain numerous meaningful community partnerships. Traditionally, community organizations have been hesitant to partner with government agencies, such as the VHA, due to histories of institutional mistrust and bureaucracy.28
The PSCI-SPC model for developing a VHA-community collaborative partnership draws from the tradition of community-based participatory research. The best community-based participatory research practices are to build on strengths and resources within the local community; develop collaborative, equitable partnerships that involve an empowering and power-sharing process; foster colearning, heuristics, and capacity building among partners; and focus on systems development using an iterative process. These practices also are consistent with the literature on learning collaboratives.29-31
The premise for a learning collaborative is to bridge the gap between knowledge and practice in health care.31 Figure 1 depicts how this collaborative was developed, and how it supports Objectives 2 and 3. To achieve Objective 1, we developed a VHA-learning collaborative of 13 influential community partners in the Denver and Colorado Springs region of Colorado. The VHA team consists of a learning collaborative leader, a program manager, and a program support assistant. The principal investigator attends and contributes to all meetings. Learning collaborative partners include a university psychology clinic that focuses on veterans’ care, 3 veterans service organizations, a mental health private practice, a university school of nursing, a community mental health center, veterans’ courts, and 5 city departments.
These partners participated in qualitative interviews to identify where gaps and breakdowns were occurring. With this information, the PSCI-SPC team and VHA-learning collaborative held a kickoff event. At this meeting the team discussed the qualitative findings, provided veteran suicide prevention information, and basic information regarding suicide prevention program building and implementation science.
Throughout quarterly learning collaborative meetings and monthly facilitation calls, we have worked to develop a blueprint and an action plan for each partner to develop best practices for dissemination to aid in providing consistency in the standard of care. A postimplementation event will be held to identify successes and challenges encountered while operationalizing project action plans.
Currently, activities of the learning collaborative are making a large impact on the community. Not all collaborative members track information regarding their populations served, nor specific metrics on veterans encountered. Even so, of those who do capture metrics, suicide prevention program components implemented by the collaborative will impact more than 21,000 individuals and at least 2,500 known veterans. In addition, 52 new connections have been made between community organizations or between community organizations and the VHA, and > 300 individuals have been trained.The learning collaborative support team has assisted in the dissemination of a large resource list for veterans. As the learning collaborative is ongoing and we are working with organizations to improve their data collection and analytics, we expect these numbers to increase. We anticipate that the learning collaborative will develop a stronger suicide prevention safety net within the community. In addition, we expect increased referrals of at-risk veterans to the VHA and enhance the long-term continuity of care between community and VHA services.