The Veterans Affairs Patient Safety Center of Inquiry—Suicide Prevention Collaborative: Creating Novel Approaches to Suicide Prevention Among Veterans Receiving Community Services
Background: While the US Department of Veterans Affairs has made significant strides to prevent veteran suicide, efforts have largely targeted veterans actively engaged in and eligible for Veterans Health Administration (VHA) care, which is consistent with the VHA mission. The majority of veterans are not enrolled in VHA care, and many are ineligible for services. Veterans not connected to VHA have experienced an increase in suicides in recent years.
Observations: Since 2018, VHA National Center for Patient Safety has funded the Patient Safety Center of Inquiry-Suicide Prevention Collaborative (PSCI-SPC), which has worked to develop, implement, and evaluate practical solutions aimed at curbing the rising suicide rate among veterans not receiving VHA care. PSCI-SPC has 3 guiding objectives: (1) Develop and test a collaborative, organizational structure to connect VHA and community organizations, such as national, local, public, private, nonprofit, and academic partners who provide high-quality and timely health care; (2) Build and test a learning collaborative to facilitate sharing of VHA suicide prevention best practices with community partners to increase availability, consistency, and quality of mental health services for all veterans; and (3) Implement, test, and refine a novel program to provide affordable suicide prevention interventions to veterans with mental health needs, regardless of their use of, or eligibility for, VHA services. This paper details the current progress for this demonstration project. As these objectives are met, PSCI-SPC will create and disseminate products to support broad implementation of these practices to other VA medical centers and the communities they are embedded in.
Conclusions: PSCI-SPC seeks to fill an important gap in veteran health care by serving as a national clinical innovation and dissemination center for best practices in suicide prevention for veterans who receive care in their communities.
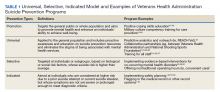
In response to the high rates of veteran suicide deaths, the US Department of Veterans Affairs (VA) has developed a broad, multicomponent suicide prevention program that is unparalleled in private US health care systems.4,7 Suicide prevention efforts are led and implemented by both the VHA National Center for Patient Safety and the VHA Office of Mental Health and Suicide Prevention. Program components are numerous and multifaceted, falling within the broad promotion and prevention strategies outlined by the National Academy of Medicine (NAM).1,8-11 The NAM continuum of prevention model encompassing multiple strategies is also referred to as the Universal, Selective, Indicated (USI) Model.7,8,10 The VHA suicide prevention program contains a wide spread of program components, making it both comprehensive and innovative (Table 1).
Although significant momentum and progress has been made within the VHA, policy set by legislation has historically limited access to VHA health care services to VHA-eligible veterans. This is particularly concerning given the rising suicide rates among veterans not engaged in VHA care.2 Adding to this complexity, recent legislation has increased veterans’ access to non-VHA health care, in addition to their existing access through Medicare, Medicaid, and other health care programs.12-14 Best practices for suicide prevention are not often implemented in the private sector; thus, these systems are ill prepared to adequately meet the suicide prevention care needs of veterans.4,15-18 Furthermore, VHA and non-VHA services generally are not well coordinated, and private sector health care providers (HCPs) are not required to complete a commensurate level of suicide prevention training as are VHA HCPs.16-18 Most non-VHA HCPs do not receive military cultural competence training.19 These issues create a significant gap in suicide prevention services and may contribute to the increases in suicide rates in veterans who do not receive VHA care. Thus, changes in policy to increase access through private sector care may have paradoxical effects on veteran suicide deaths. To impact the veteran suicide rate, VHA must develop and disseminate best practices for veterans who use non-VHA services.
A Roadmap to Suicide Prevention
There is significant momentum at the federal level regarding this issue. The President’s Roadmap to Empower Veterans and End the National Tragedy of Suicide (Executive Order 13,861) directs the VHA to work closely with community organizations to improve veteran suicide prevention.20 The VHA and partners, such as the Substance Abuse and Mental Health Services Administration (SAMHSA), are bridging this gap with collaborative efforts that increase suicide prevention resources for veterans living in the community through programs such as the Governor’s Challenges to Prevent Suicide Among Service Members, Veterans, and their Families. These programs intend to empower communities to develop statewide, strategic action plans to prevent veteran suicide.7,21-24
In addition to partnerships, VHA has built other aspects of outreach and intervention into its programming. A key VHA initiative is to “know all veterans” by committing to identifying and reaching out to all veterans who may be at risk for suicide.22 The VHA has committed to offering “emergency stabilization care for former service members who present at the facility with an emergent mental health need” regardless of eligibility.25 The intent is to provide temporary emergent mental health care to veterans who are otherwise ineligible for care, such as those who were discharged under other-than-honorable conditions while the VHA determines eligibility status.26 However, veterans must meet certain criteria, and there is a limit on services.
Although services are being expanded to reach veterans who do not access VHA health care, how to best implement these new directives with regard to suicide prevention is unclear. Strategic development and innovations to expand suicide prevention care to veterans outside the current reach of VHA are desperately needed.