Implementation of a Pharmacist-Managed Transitions of Care Tool
Purpose: To improve, expand, and sustain a pharmacist-based transitions of care (TOC) program and to assess interventions targeting veterans at high risk for adverse outcomes.
Methods: A TOC program was developed and piloted at the Richard L. Roudebush Veterans Affairs Medical Center (RLRVAMC). Following success of the pilot project, targeted interventions were identified to improve and expand the program. Patients deemed high risk for readmission by an acute care pharmacist were identified and referred for continued postdischarge follow-up. The study population included patients discharged to the community with primary care established within the RLRVAMC system. Eligible patients were entered into a TOC database by the referring acute care pharmacist. A pharmacist in the primary care clinic reviewed then contacted the patient within 1 week of discharge. Appropriate documentation of each visit was completed in the electronic health record. Data collection included background information, time to follow-up, medication discrepancies, pharmacist interventions, emergency department visits, and hospital readmissions.
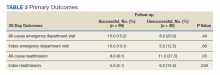
Results: A total of 139 patients were included, of which 99 patients were reached for pharmacist follow-up. There were 43 medication-related discrepancies among all patients. The most common discrepancy was taking the wrong dose of a prescribed medication. Additional counseling was provided to 75% of patients. The subset of patients who were reached by a pharmacist had decreased index (5.1% vs 15.0%; P = .049) and all-cause readmissions (8.1% vs 27.5%; P = .03) at 30 days compared with those who did not received pharmacist follow-up, respectively.
Conclusions: This study demonstrated that implementation and expansion of a pharmacist-based TOC process is effective in communicating high-risk patients and intervening on medication-related issues postdischarge.
Program Referrals
After expansion to include the VA CBOCs, elimination of the elevated LACE or CAN score requirement, and additional staff education, the rate of referrals per month increased during phase 2 in comparison to the pilot study (Figure 3). There were a mean (SD) of 34 (10) referrals per month. Although not statistically analyzed, it is an objective increase in comparison to a mean 19 referrals per month in the pilot study.
Discussion
The continued development and use of a pharmacist-driven TOC tool at RLRVAMC increased communication and follow-up of high-risk patients, demonstrated the ability of pharmacists to identify and intervene in medication-related issues postdischarge, and successfully reduce 30-day readmissions. This program emphasized pharmacist involvement during the discharge process and created a standardized mechanism for TOC follow-up, addressing multiple areas that were identified by The Joint Commission as being associated with poor outcomes. The advanced pharmacy practice model at RLRVAMC allowed for a multidimensional program, including prospective patient identification and multiple pharmacy touchpoints. This is unique in comparison to many of the one-dimensional programs described in the literature.
Polypharmacy has been identified as a major predictor of medication discrepancies postdischarge, and patients with ≥ 10 active medications have been found to be at highest risk.13,14 Patients in this study had a mean 13 active medications on admission, with a mean 5 medication changes at discharge. PACT pharmacists documented 28 of 99 patients with ≥ 1 medication-related discrepancy at postdischarge reconciliation. This 28% discrepancy rate is consistent with discrepancy rates previously reported in the literature, which ranged from 14 to 45% in large meta-analyses.14,15 The majority of these discrepancies (58%) were related to patients who took the wrong dose of a prescribed medication.
Targeted interventions to overcome barriers in the pilot study increased the referral rates to the TOC tool; however, the increase in referral rate was associated with increased time to follow up by ambulatory care pharmacists. The extended follow-up times were seen most often in the 2 busiest primary care clinics, one of which is considered a teaching clinic for medical residents. Pharmacists were required to integrate these calls into their normal work schedule and were not provided additional time for calling, allowing for an increased follow-up time. The increased follow-up time likely contributed to the increased number of patients excluded due to already having PACT follow-up, giving more time for the primary care provider to have an appointment with the patient. The ambulatory care pharmacist could then determine whether further intervention was needed. In the summer of 2018, a decrease in referral rates occurred for a short time, but this is likely explained by incoming new residents and staff within the pharmacy department and decreased awareness among the new staff. The enhanced staff education took place during September 2018 and lead to increased referral rates compared with those seen in months prior.
PACT pharmacists were not only able to identify discrepancies, but also provide timely intervention on a multitude of medication-related issues by using their scope of practice (SOP). Most interventions were related to medication or disease counseling, including lifestyle, device, and disease education. The independent SOP of our PACT pharmacists is a unique aspect of this program and allowed pharmacists to independently adjust many aspects of a patient’s medication regimen during follow-up visits.
The outcomes of 30-day index and all-cause readmissions, as well as index and all-cause ED visit rates, were lower in the subset of patients who received PACT pharmacist follow-up after discharge (Table 3). The difference was most pronounced in the all-cause readmission rates: Only 8.1% of patients who received PACT follow-up experienced a readmission compared with 27.5% of those who did not. The difference between the groups regarding ED visit rates were not as pronounced, but this may be attributed to a limited sample size. These data indicate that the role of the pharmacist in identifying discrepancies and performing interventions at follow-up may play a clinically significant part in reducing both ED visit rates and hospital readmissions.