Implementation of a Pharmacist-Managed Transitions of Care Tool
Purpose: To improve, expand, and sustain a pharmacist-based transitions of care (TOC) program and to assess interventions targeting veterans at high risk for adverse outcomes.
Methods: A TOC program was developed and piloted at the Richard L. Roudebush Veterans Affairs Medical Center (RLRVAMC). Following success of the pilot project, targeted interventions were identified to improve and expand the program. Patients deemed high risk for readmission by an acute care pharmacist were identified and referred for continued postdischarge follow-up. The study population included patients discharged to the community with primary care established within the RLRVAMC system. Eligible patients were entered into a TOC database by the referring acute care pharmacist. A pharmacist in the primary care clinic reviewed then contacted the patient within 1 week of discharge. Appropriate documentation of each visit was completed in the electronic health record. Data collection included background information, time to follow-up, medication discrepancies, pharmacist interventions, emergency department visits, and hospital readmissions.
Results: A total of 139 patients were included, of which 99 patients were reached for pharmacist follow-up. There were 43 medication-related discrepancies among all patients. The most common discrepancy was taking the wrong dose of a prescribed medication. Additional counseling was provided to 75% of patients. The subset of patients who were reached by a pharmacist had decreased index (5.1% vs 15.0%; P = .049) and all-cause readmissions (8.1% vs 27.5%; P = .03) at 30 days compared with those who did not received pharmacist follow-up, respectively.
Conclusions: This study demonstrated that implementation and expansion of a pharmacist-based TOC process is effective in communicating high-risk patients and intervening on medication-related issues postdischarge.
Methods
Phase 2 was a quality improvement initiative; therefore, institutional review board approval was not needed. The aim of phase 2 was to improve, expand, and sustain the TOC program that was implemented in the pilot study. Barriers identified after discussion with acute care and PACT pharmacists included difficulty in making referrals due to required entry of cumbersome readmission risk factor calculations, limiting inclusion to patients who receive primary care at the main hospital facility, and the expansion of pharmacy staff with new pharmacists who were not knowledgeable of the referral process.
Design
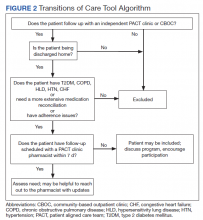
To overcome barriers, 4 main targeted interventions were needed: streamlining the referral process, enhancing pharmacy staff education, updating the discharge note template, and expanding the criteria to include patients who receive care at VA CBOCs. The referral process was streamlined by removing required calculated readmission risk scores, allowing pharmacist judgement to take precedence for referrals. Focused face-to-face education was provided to acute care and PACT pharmacists about the referral process and inclusion criteria to increase awareness and provide guidance of who may benefit from entry into the tool. Unlike the first phase of the study, education was provided for outpatient staff pharmacists responsible for discharging patients on the weekends. Additionally, the pharmacists received a printed quick reference guide of the information covered during the education sessions (Figure 2). Referral prompts were embedded into the standard pharmacy discharge note template to serve as a reminder to discharging pharmacists to assess patients for inclusion into the tool and provided a direct link to the tool. Expansion to include VA CBOCs occurred postpilot study, allowing increased patient access to this TOC service. All other aspects of the program were continued from the pilot phase.
Patients were eligible if they were discharged from RLRVAMC between October 1, 2018 and February 28, 2019. Additionally, the patient had to be established in a PACT clinic for primary care and have been referred to the tool based on the discretion of an acute care pharmacist. Patients were excluded if they were discharged against medical advice or to any facility where the patient and/or caregiver would not be responsible for medication administration (eg, subacute rehabilitation, extended care facility), or if the patient refused pharmacy follow-up.
Outcomes
The primary outcomes assessed were all-cause and index ED visits and readmissions within 30 days of discharge. All-cause ED visits and readmissions were defined as a second visit to RLRVAMC , regardless of readmission diagnosis. Index ED visits and readmissions were defined as those that were related to the initial admission diagnosis. Additional data collected and analyzed included the number of patients referred by pharmacists, number and type of medication discrepancies, medication changes, counseling interventions, time to follow-up postdischarge, and number of patients added to the PACT pharmacist’s clinic schedule for further management. A discrepancy identified by a PACT pharmacist was defined as a difference between the discharge medication list and the patient-reported medication list at the time of follow-up. Patients who were referred to the TOC tool but were unable to be reached by telephone served as the control group for this study.