Glioblastoma: Prognosis is poor, but new therapies are emerging
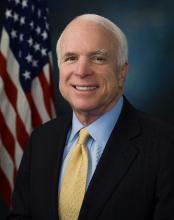
The questioning of former FBI director James B. Comey by Sen. John McCain (R-Ariz.) during a June 8 Senate Intelligence Committee hearing raised more than a few eyebrows; Sen. McCain seemed confused and disoriented, at one point referring to Mr. Comey as “President Comey,” but a possible medical explanation emerged soon after.
On July 14, Sen. McCain, 80, underwent surgery to remove a 5-cm blood clot that had been discovered above his left eye during a physical, and on July 19, the Mayo Clinic in Phoenix, where he had undergone the procedure, announced at his request that, “subsequent tissue pathology revealed that a primary brain tumor known as a glioblastoma was associated with the blood clot.”
Glioblastoma features
While Sen. McCain’s symptoms can’t necessarily be attributed to the glioblastoma, it is not unusual for glioblastoma patients to present with some sort of neurologic deficit, such as speech issues, unilateral weakness, or confusion, according to Eudocia Quant Lee, MD, a neuro-oncologist at Dana-Farber Cancer Institute, Boston.
Neuro-oncologist Manmeet Singh Ahluwalia, MD, of the Cleveland Clinic said seizures, persistent headaches, double or blurred vision, and changes in ability to think and learn can also be presenting symptoms.
Glioblastoma is the most common malignant primary brain tumor diagnosed in adults, with an estimated 12,000-13,000 new cases occurring each year in the United States. It is more common among older adults but can occur in younger patients. It arises in the brain and generally stays within the central nervous system, Dr. Lee explained, noting that it is much less common than lung cancer, breast cancer, and melanoma.
This is particularly true for older patients.
Prognosis and age
“We know, in general – as with most cancers – that the older you’re diagnosed with your cancer, the poorer your prognosis is,” she said, adding that other health issues and the ability to tolerate treatment can affect outcomes.
Outcomes also can be affected by type of surgery, functional status, extent of treatment, and molecular subtypes of the glioblastoma, Dr. Ahluwalia said.
Survival generally ranges about 14-18 months, although about 10% of patients live 5 years or longer.
The study, presented in a poster by Michael Weller, MD, of University Hospital and University of Zürich and his colleagues, also showed that, compared with the 398 older patients who survived less than 2 years (median, 6.2 months), those who survived longer had “more intensive up-front treatment and a trend toward higher initial Karnofsky performance scores as distinguishing clinical factors.”
In addition, molecular analyses showed more frequent O6-methylguanine-DNA methyltransferase (MGMT) promoter methylation in those with longer survival, while isocitrate dehydrogenase (IDH) mutations were restricted to single patients.
“Collectively, our findings confirm that LTS is rare in elderly patients with glioblastoma and that clinical and tumor-associated molecular factors linked to LTS resemble those in standard-age patients, except for less common IDH mutation,” the investigators wrote.
Another abstract published online in conjunction with the ASCO annual meeting looked at outcomes, based on age and MGMT analysis, and similarly found that aggressive treatment with chemoradiation is associated with better outcomes in both younger and older patients.
In that study by Suryanarayan Mohapatra, MD, of Cleveland Clinic–Fairview Hospital, and his colleagues – including Dr. Ahluwalia – 567 of 1,165 patients were aged 65 years or older. The benefits of chemoradiation therapy, which was associated with a significantly lower risk of death vs. radiation therapy alone in the study, were more pronounced among the older patients (hazard ratio, 0.45 vs. 0.61 for those under age 65 years), but the difference did not reach statistical significance.
Dr. Mohapatra and his colleagues also showed that more aggressive therapy resulted in better overall and progression-free survival regardless of MGMT methylation status, but that there was no difference between the age groups on this measure. Overall and progression-free survival also were significantly better with gross-total resection and subtotal resection vs. biopsy only, and with diagnosis during 2009 and later vs. during 2007-2008. However, a difference between the two age groups was seen with respect to overall survival only among those diagnosed during 2009 or later, with a more prominent impact among the younger group, the investigators reported.
“Older individuals often get less aggressive treatment. However, based on the research, active and functional older patients should get aggressive treatment,” Dr. Ahluwalia said. “We advocate tailor-made treatment that takes into account patient condition, location of tumor, functional status, etc., in addition to patient age.”