Physician Responsiveness to Positive Blood Culture Results at the Minneapolis Veterans Affairs Hospital—Is Anyone Paying Attention?
Background: Patients presenting with suspected infections are typically placed on empiric broad-spectrum antibiotics. With mounting evidence supporting the efficacy of using the narrowest spectrum of antimicrobial therapy to cover the suspected pathogen, current guidelines recommend decreasing the breadth of coverage in response to culture results both in relation to microbe identification and antibiotic sensitivity.
Methods: A retrospective chart review of electronic health records at the Minneapolis Veterans Affairs Medical Center (VAMC) in Minnesota was performed for 208 positive blood cultures with antibiotic spectrum analysis from July 1, 2015 to June 30, 2016. The time of reporting for pathogen identification and subsequent pathogen susceptibilities were compared to the time at which any alterations to antibiotic coverage were made. The breadth of antibiotic coverage was recorded using a nonlinear spectrum score. The use of this score allowed for the reliable classification of antibiotic adjustments as either deescalation, escalation, or no change.
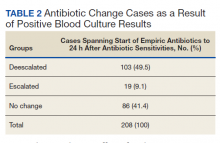
Results: The percentage of cases deescalated was higher in response to physician (house staff or attending physician) notification of pathogen susceptibility information when compared with a response to pathogen identification alone (33.2% vs 22.6%). Empiric antibiotics were not altered within 24 hours in response to pathogen identification in 70.7% of cases and were not altered within 24 hours in response to pathogen sensitivity determination in 58.6% of cases. However, when considering the time frame from when empiric antibiotics were started to 24 hours after notification of susceptibility information, 49.5% of cases were deescalated and 41.5% of cases had no net change in the antibiotic spectrum score. The magnitude of deescalations were notably larger than escalations. The mean (SD) time to deescalation of antibiotic coverage was shorter ( P =.049) in response to pathogen identification at 8 (7.4) hours compared with sensitivity information at 10.4 (7) hours, but may not be clinically relevant.
Conclusion: Health care providers at the Minneapolis VAMC appear to be using positive blood culture results in a timely fashion consistent with best practices. Because empirically initiated antibiotics typically are broad in spectrum, the magnitude of deescalations were notably larger than escalations. Adherence to these standards may be a reflection of the infectious disease staff oversight of antibiotic administration. Furthermore, the systems outlined in this quality improvement study may be replicated at other VAMCs across the country by either in-house infectious disease staff or through remote monitoring of the electronic health record by other infectious disease experts at a more centralized VAMC. Widespread adoption throughout the Veterans Health Administration may result in improved antibiotic resistance profiles and better clinical outcomes for our nation’s veterans
Discussion
The strategy of the infectious disease team at MVAMC is one of deescalation. One challenge of quantifying deescalation was to make a reliable and agreed-upon definition of just what deescalation entails. In 2003, the pharmaceutical company Merck was granted a trademark for the phrase “De-Escalation Therapy” under the international class code 41 for educational and entertainment services. This seemed to correspond to marketing efforts for the antibiotic imipenem/cilastatin. Although the company trademarked the term, it was never defined. The usage of the phrase evolved from a reduction of the dosage of a specific antibiotic to a reduction in the number of antibiotics prescribed to that of monotherapy. The phrase continues to evolve and has now become associated with a change from combination therapy or broad-spectrum antibiotics to monotherapy, switching to an antibiotic that covers fewer pathogens, or even shortening the duration of antibiotic therapy.34 The trademark expired at about the same time the imipenem/cilastatin patent expired. Notably, this drug had initially been marketed for use in empiric antibiotic therapy.35
Barriers
The goal of the stewardship program was not to see a narrowing of the antibiotic spectrum in all patients. Some diseases such as diverticulitis or diabetic foot infections are usually associated with multiple pathogens where relatively broad-spectrum antibiotics seem to be preferred.36,37 Heenen and colleagues reported that infectious disease specialists recommended deescalation in < 50% of cases they examined.38
Comparing different institutions’ deescalation rates can be confusing due to varying definitions, differing patient populations, and health care provider behavior. Thus, the published rates of deescalation range widely from 10 to 70%.2,39,40 In addition to the varied definitions of deescalation, it is challenging to directly compare the rate of deescalation between studies due to institutional variation in empirical broad-spectrum antibiotic usage. A hospital that uses broad-spectrum antibiotics at a higher rate than another has the potential to deescalate more often than one that has low rates of empirical broad-spectrum antibiotic use. Some studies use a conservative definition of deescalation such as narrowing the spectrum of coverage, while others use a more general definition, including both the narrowing of spectrum and/or the discontinuation of antibiotics from empirical therapy.41-45 The more specific and validated definition of deescalation used in this study may allow for standardized comparisons. Another unique feature of this study is that all positive blood cultures were followed, not only those of a particular disease.
One issue that comes up in all research performed within the VA is how applicable these results are to the general public. Nevertheless, the stewardship program as it is structured at the MVAMC could be applied to other non-VA institutions. We recognize, however, that some smaller hospitals may not have infectious diseases specialists on staff. Despite limited in-house staff, the same daily monitoring can be performed off-site through review of the EHR, thus making this a viable system to more remote VA locations.
While deescalation remains the standard of care, there are many complexities that explain low deescalation rates. Individual considerations that can cause physicians to continue the empirically initiated broad-spectrum coverage include differing renal toxicities, suspecting additional pathogens beyond those documented in testing results, and differential Clostridium difficile risk.46,47 A major concern is the mind-set of many prescribers that streamlining to a different antibiotic or removing antibiotics while the patient is clinically improving on broad empiric therapy represents an unnecessary risk.48,49 These thoughts seem to stem from the old adage, “If it ain’t broke, don’t fix it.”
Due to the challenges in defining deescalation, we elected to use a well-accepted and validated methodology of Madaras-Kelly.33 We recognize the limitations of the methodology, including somewhat differing opinions as to what may constitute breadth and narrowing among clinicians and the somewhat arbitrary assignment of numerical values. This tool was developed to recognize only relative changes in antibiotic spectrum and is not quantitative. A spectrum score of piperacillin/tazobactam of 42.3 could not be construed as 3 times as broad as that of vancomycin at 13. Thus, we did not perform statistical analysis of the magnitude of changes because such analysis would be inconsistent with the intended purpose of the spectrum score method. Additionally, while this method demonstrated reliable classification of appropriate deescalation and escalation in previous studies, a case-by-case review determining appropriateness of antibiotic changes was not performed.
Clinical Response
This quality improvement study was initiated to determine whether positive blood culture results actually affect clinical management at MVAMC. The answer seems to be yes, with blood culture results altering antibiotic administration in about 60% of cases with the predominant change being deescalation. This overall rate of deescalation is toward the higher end of previously documented rates and coincides with the upper bound of the clinically advised deescalation rate described by Heenen and colleagues.38
As noted, the spectrum score is not quantitative. Still, one may be able to contend that the values may provide some insight into the magnitude of the changes in antibiotic selection. Deescalations were on average much larger changes in spectrum than escalations. The larger magnitude of deescalations reflects that when already starting with a very broad spectrum of coverage, it is much easier to get narrower than even broader. Stated another way, when starting therapy using piperacillin/tazobactam at a spectrum score of 42.3 on a 60-point scale, there is much more room for deescalation to 0 than escalation to 60. Additionally, escalations were more likely with much smaller of a spectrum change due to accurate empirical judgment of the suspected pathogens with new findings only necessitating a minor expansion of the spectrum of coverage.