Get ready for a practice makeover
HPV vaccine imminent … Colposcopy disappoints … LEEP raises preterm risk … LSIL meaningless?
Although Consensus Guidelines state that both ablative and excisional methods are acceptable forms of managing women with satisfactory colposcopy and CIN 2,3, for most clinicians, LEEP has completely replaced laser ablation and cryotherapy for treatment of CIN.1 Because LEEP is so widely utilized, its effects on fertility and preterm delivery, as well as other adverse pregnancy outcomes, are of great concern.
LEEP became widely adopted since its introduction in the early 1990s because it yields a tissue specimen for histological evaluation and is less expensive and easier to perform than laser ablation.
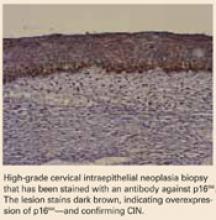
Many consider CIN 2,3 biomarkers the next step away from the Pap smear, toward more accurate molecular testing. One of the more promising biomarkers is p16INK4A, a cyclin-dependent kinase inhibitor involved in control of the cell cycle. Wang et al took tissue blocks from a large population-based screening study and evaluated the performance of p16INK4A on the full diagnostic spectrum of lesions. A very strong correlation was seen between identification of p16INK4A in the lesion and CIN 2,3; 100% of CIN 3 lesions showed diffuse staining with p16INK4A.
Wang S, Trunk M, Schiffman, M et al. Validation of p16INK4a as a marker of oncogenic human papillomavirus infection in cervical biopsies from a population-based cohort in Costa Rica. Cancer Epidemiol Biomarkers Prev. 2004;13:1355–1360.
Unfortunately, most studies of the impact of LEEP on fertility and pregnancy have been limited or inconclusive, and most lacked statistical power to detect a doubling of risk. The New Zealand study conducted by Sadler and colleagues—a large retrospective cohort study—compared delivery outcomes of 426 untreated women with 652 women treated by laser conization, laser ablation, or LEEP. Women who had LEEP or laser cone treatment were at significantly increased risk of rupture of membranes before 37 weeks’ gestation. Notably, in women who had undergone a LEEP, the adjusted relative risk (RR) for PPROM was 1.9 (95% CI, 1.0-3.8) compared to the untreated women. Laser ablation did not increase risk (RR 1.1). This study demonstrate that women who have undergone LEEP have almost twice the risk for PPROM as untreated women, should be of concern to all gynecologists.
Risk of both PPROM and preterm delivery increased as depth of cervical tissue removed increased. Women in whom 1 cm or less of tissue was excised had no increased risk of PPROM or preterm birth; women in whom more than 1.7 cm of tissue was excised had an adjusted relative risk of 3.6 (95% CI, 1.8-7.5).
In a Canadian study published only last month, Samson and colleagues found PPROM was almost 4 times more common among women who had had a LEEP.2
REFERENCES
1. Wright TC, Jr, Cox JT, Massad LS, Carlson J, Twiggs LB, Wilkinson EJ. 2001 consensus guidelines for the management of women with cervical intraepithelial neoplasia. Am J Obstet Gynecol. 2003;189:295-304.
2. Samson S, Bentley JR, Fahey T, McKay D, Gill G. The effect of loop electrosurgical excision procedure on future pregnancy outcome. Obstet Gynecol. 2005;105:325-332.
LSIL cytology meaningless?
Moscicki A, Shiboski S, Hills N, et al. Regression of low-grade squamous intraepithelial lesions in young women. Lancet. 2004;364:1678–1683.
This study shows just how meaningless LSIL cytology is in young women—and it portends changes in the next Consensus Guidelines. Colposcopy for all adolescents and young women is unwarranted, the authors stated. They recommend monitoring with repeat cytology instead.
For over a decade it has been widely appreciated that many CIN 1 lesions spontaneously regress in the absence of therapy.1 Based on what we recently learned from natural history studies of HPV, we know that the majority of LSIL cytology results and biopsy-confirmed CIN 1 lesions represent nothing more than the morphological manifestation of a productive HPV infection.2 HPV infections, including those with high-risk types of HPV, are typically self-limited (FIGURE 2). In approximately 90% of women, HPV shedding stops spontaneously within 24 months.
However, in the United States, most women with LSIL undergo colposcopy, and many clinicians continue to treat women with biopsy-confirmed CIN 1. These approaches do correspond to the most recent Consensus Guidelines, which recommend colposcopy for women with LSIL, and state that follow-up with treatment, as well as treatment with ablative or excisional methods, are acceptable management options for women with CIN 1.3
Regarding adolescents with LSIL, the guidelines made an exception to performing a colposcopy. For these patients, an acceptable management option is follow-up without initial colposcopy, using a protocol of repeat cytological testing at 6 and 12 months, or HPV testing at 12 months.