Shifting Culture Toward Age-Friendly Care: Lessons From VHA Early Adopters
Background: The need for a health care workforce with expanded skills in the care of older adults is increasingly evident as the US population ages. The evidence-based Age-Friendly Health Systems (AFHS) framework establishes a structure to reliably assess and deliver effective care of older adults with multiple chronic conditions: what matters, medication, mentation, and mobility (4Ms). Half of veterans receiving Veterans Health Administration (VHA) care are aged ≥ 65 years, driving its transformation into the largest AFHS in the US. In this article, we offer lessons on the challenges to AFHS delivery and suggest opportunities to sustaining age-friendly care.
Observations: Within 3 months of implementation, 85% to 100% of patients received 4M care in all care settings at our VA facilities. Key lessons learned include the importance of identifying, preparing, and supporting a champion to lead this effort; garnering facility and system leadership support at the outset; and integration with the electronic health record (EHR) for reliable and efficient data capture, reporting, and feedback. Although the goal is to establish AFHS in all care settings, we believe that initially including a geriatrics-focused care setting helped early adoption of 4Ms care in the sites described here.
Conclusions: Early adopters at 2 VHA health care systems demonstrated successful AFHS implementation spanning different VHA facilities and care settings. Successful growth and sustainability may require leveraging the EHR to reduce documentation burden, increase standardization in care, and automate feedback, tracking, and reporting. A coordinated effort is underway to integrate AFHS into VHA documentation, performance evaluation, and metrics in both the legacy and new Cerner EHRs.
Step 5: Study Performance
The IHI identifies 3 methods for measuring older adults who receive 4Ms care: real-time observation, chart review, or EHR report. For chart review, the IHI recommends using a random sample to calculate the number of patients who received 4Ms in 1 month, which provides evidence of progress toward reliable practice.
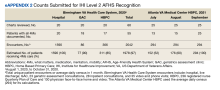
Both facilities used chart review with random sampling. Each setting estimated the number of veterans receiving 4Ms care by multiplying the percentage of sampled charts with documented 4Ms care by unique patient encounters (eAppendix 2).
From August through October 2020, BVAHCS sites reached an estimated 97% of older veterans with complete 4Ms care: hospital, 100%; GAC, 90%; and HBPC, 85%. AVAMC HBPC increased 4Ms care from 52% to 100% between July and September 2021. Both teams demonstrated the feasibility of reliably providing 4Ms care to > 85% of older veterans in these care settings and earned level 2 recognition. Through satisfaction surveys and informal feedback, notable positive changes were evident to veterans, their families, and the VA staff providing 4Ms age-friendly care.
Step 6: Improve and Sustain Care
Each site acknowledged barriers and facilitators for adopting the 4Ms. The COVID-19 pandemic was an ongoing barrier for both sites, with teams transitioning to virtual modalities for telehealth visits and team meetings, and higher staff turnover. However, the greater use of technology facilitated 4Ms adoption by allowing physically distant team members to collaborate.
One of the largest barriers was the lack of 4Ms documentation in the EHR, which could not be implemented in the BVAHCS inpatient hospital due to existing standardized nursing templates. Both sites recognized that 4Ms documentation in the EHR for all care settings would facilitate achieving level 2 recognition and tracking and reporting 4Ms care in the future.
Discussion
The AFHS 4Ms approach offers a method to impart geriatrics knowledge, skills, and practice throughout an entire health care system in a short time. The AFHS framework provides a structured pathway to the often daunting challenge of care for complex, multimorbid, and highly heterogeneous older adults. The 4Ms approach promotes the provision of evidence-based care that is reliable, efficient, patient centered, and avoids unwanted care: worthy goals not only for geriatrics but for all members of a high-reliability organization.
Through the implementation of the 4Ms framework, consistent use of AFHS practices, measurement, and feedback, the staff in each VA care setting reported here reached a level of reliability in which at least 85% of patients had all 4Ms addressed. Notably, adoption was strong and improvements in reliably addressing all 4Ms were observed in both geriatrics (HBPC and outpatient clinics) and nongeriatrics (inpatient medicine) settings. Although one might expect that high-functioning interdisciplinary teams in geriatrics-focused VA settings were routinely addressing all 4Ms for most of their patients, our experience was consistent with prior teams indicating that this is often not the case. Although many of these teams were addressing some of the 4Ms in their usual practice, the 4Ms framework facilitated addressing all 4Ms as a set with input from all team members. Most importantly, it fostered a culture of asking the older adult what matters most and documenting, sharing, and aligning this with the care plan. Within 6 months, all VA care settings achieved level 1 recognition, and within 9 months, all achieved level 2 recognition.