A Case Series of Rare Immune-Mediated Adverse Reactions at the New Mexico Veterans Affairs Medical Center
Background: Immune checkpoint inhibitor (ICI) therapy has revolutionized the treatment of several solid tumors. The use of ICIs is expected to rise as a growing number of indications are approved for their use by the US Food and Drug Administration and with the increasing number of patients with cancer. Unfortunately, ICIs are associated with the development of immune-mediated adverse reactions (IMARs). About 5% to 10% of patients developing severe toxicities requiring treatment postponement or discontinuation. IMARs can affect any organ, but most frequently the skin and endocrine glands are involved.
Case Presentation: We present a case series of IMARs observed at the New Mexico Veterans Affairs Medical Center. First, we present a case of grade 4 myocarditis in an 84-year-old man receiving chemoimmunotherapy for lung adenocarcinoma to demonstrate the rapid progression of this rare condition. Second, we present a case of uveitis in a 70-year-old man with superficial bladder cancer undergoing treatment with pembrolizumab. Finally, we present a case of a 63-year-old man with pleuritis and organizing pneumonia secondary to dual ICI treatment (nivolumab and ipilimumab) for mesothelioma. A discussion regarding the epidemiology of these IMARs, expected course, and optimal management follows each rare toxicity described.
Conclusions: Though these toxicities are uncommon, they serve as a reminder to clinicians across specialties that IMARs can drive the acute deterioration of any organ, and consideration of toxicities secondary to ICIs should be considered for any atypical presentation of unclear etiology.
Case 2: Uveitis
A 70-year-old man who received pembrolizumab as a bladder-sparing approach for his superficial bladder cancer refractory to intravesical treatments developed uveitis. Approximately 3 months following the initiation of treatment, the patient reported bilateral itchy eyes, erythema, and tearing. He had a known history of allergic conjunctivitis that predated the ICI therapy, and consequently, it was unclear whether his symptoms were reflective of a more concerning issue. The patient’s symptoms continued to wax and wane for a few months, prompting a referral to ophthalmology colleagues at NMVAMC.
Ophthalmology evaluation identified uveitic glaucoma in the setting of his underlying chronic glaucoma. Pembrolizumab was discontinued, and the patient was counseled on choosing either cystectomy or locoregional therapies if further tumors arose. However, within a few weeks of administering topical steroid drops, his symptoms markedly improved, and he wished to be restarted on pembrolizumab. His uveitis remained in remission, and he has been treated with pembrolizumab for more than 1 year since this episode. He has had no clear findings of superficial bladder cancer recurrence while receiving ICI therapy.
Discussion
Uveitis is a known complication of pembrolizumab, and it has been shown to occur in 1% of patients with this treatment.13,14 It should be noted that most of the studies of this IMAR occurred in patients with metastatic melanoma; therefore the rate of this condition in other patients is less understood. Overall, ocular IMARs secondary to anti-PD-1 and anti-PD-L1 therapies are rare.
The most common IMAR is surface ocular disease, consisting of dry eye disease (DED), conjunctivitis, uveitis, and keratitis. Of these, the most common ocular surface disease is DED, which occurred in 1% to 4% of patients treated with ICI therapy; most of these reactions are mild and self-limiting.15 Atezolizumab has the highest association with ocular inflammation and ipilimumab has the highest association with uveitis, with reported odds ratios of 18.89 and 10.54, respectively.16 Treatment of ICI-induced uveitis generally includes topical steroids and treatment discontinuation or break.17 Oral or IV steroids, infliximab, and procedural involvement may be considered in refractory cases or those initially presenting with marked vision loss. Close communication with ophthalmology colleagues to monitor visual acuity and ocular pressure multiple times weekly during the acute phase is required for treatment titration.
Case 3: Organizing Pneumonia
A man aged 63 years was diagnosed with malignant mesothelioma after incidentally noting a pleural effusion and thickening on routine low-dose computed tomography surveillance of pulmonary nodules. A biopsy was performed and was consistent with mesothelioma, and the patient was started on nivolumab (PD-1 inhibitor) and ipilimumab (CTLA-4 inhibitor). The patient was initiated on dual ICIs, and after 6 months of therapy, he had a promising complete response. However, after 9 months of therapy, he developed a new left upper lobe (LUL) pleural-based lesion (Figure 2A).
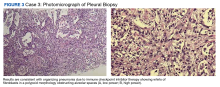
A biopsy was performed, and the histopathologic appearance was consistent with organizing pneumonia (OP) (Figure 3).