Impact of an Educational and Laboratory Stewardship Intervention on Inpatient COVID-19 Therapeutics at a Veterans Affairs Medical Center
Background: Accurate and timely prescriptions of COVID-19 therapeutics, laboratory testing, and antimicrobial stewardship have been a challenge throughout the pandemic as new evidence emerges. While universal consultation with infectious disease specialists on patients admitted with COVID-19 is desirable, it is not always feasible due to limited resources.
Observations: In this single-center study, we implemented a combined educational and laboratory stewardship intervention geared toward hospitalist practitioners resulting in improved accuracy of remdesivir and dexamethasone prescriptions, reduced laboratory use of blood cultures, interleukin 6 assay, and Legionella sputum cultures, and a decrease in antibiotic use for patients with mild-to-moderate oxygen requirements over 6 months. These improvements were seen in tandem with decreased reliance on infectious disease consultation.
Conclusions: These efforts support proof of the principle of combined educational and laboratory stewardship interventions to improve the care of COVID-19 patients, especially where infectious disease consultation may not be available or is accessed remotely.
Individual patient-level data were extracted to calculate monthly percentages of ID consultations for COVID-19 by the hospitalist team, adherence to institutional guidelines for dexamethasone and remdesivir prescriptions, and empiric antibiotic prescriptions for patients with COVID-19, including use of a priori adjudication criteria to determine justified vs unjustified empiric use. These criteria included asymmetric chest X-ray infiltrates concerning for bacterial pneumonia; peripheral white blood cell count > 11 K/μL; critical respiratory failure in the emergency department (ED) and being transferred to the ICU; and ID consultation recommended. Because the total number of antibiotics was not being analyzed but rather just the use of antibiotics for the justified and unjustified groups, antibiotic days were reported as the length of therapy (LOT).10 A subset analysis was performed on antibiotic prescriptions by the hospitalist group focusing on those with mild-to-moderate oxygen requirements (no high flow, noninvasive or invasive ventilatory methods) and excluding infections with a proven microbiologic entity.
Differences in demographic and clinical characteristics of patients with COVID-19 admitted from October 1, 2020, to March 31, 2021, were assessed using ANOVA, χ2, and Kruskal-Wallis test. χ2 was used to compare the difference in total laboratory orders for routine blood cultures, IL-6 levels, and Legionella sputum cultures between pre-intervention (October to December 2020) and postintervention (January to March 2021). These pre- and postintervention periods were determined based on the timing of revised admission orders in the EHR and initiation of focused educational sessions starting in late December 2020 and early January 2021. Linear regressions were used to examine the possible 6-month trend of the percentage of patients receiving ID consultation for appropriate dexamethasone prescriptions, appropriate remdesivir prescriptions, appropriate antibiotic coadministration, and mean number of antibiotic days per patient. Linear and logistic regression were also used to assess the trend in LOS over the 6 months while adjusting for age, race and ethnicity, sex, and coinfections. All analyses were performed using SAS 9.4. Statistical significance was defined as P < .05.
RESULTS
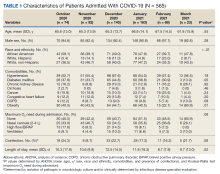
From October 1, 2020, to March 31, 2021, there were 565 admissions for COVID-19, which peaked in January 2021 with 163. Analysis of the patient characteristics showed no statistically significant difference for age, sex, oxygen requirements during admission, or proven presence of coinfection between the months of interest (Table 1).
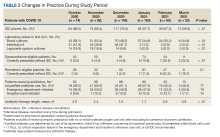
The number of blood cultures obtained in the first 24 hours of admission significantly decreased from 58.1% of admissions in October 2020 to 34.8% of admissions in March 2021 (P < .01) (Table 2).
We observed trends that coincided with the educational efforts. The rate of dexamethasone and remdesivir prescriptions for eligible patients that followed guidelines without ID consultation grew from 0% to 22.2% (P < .01) and 0% to 16.7% (P = .01), respectively. The remaining correct prescriptions for dexamethasone or remdesivir were instituted only after ID consultation. These improvements were seen in tandem with decreased reliance on ID consultation for admitted patients with COVID-19 overall (86.5% in October 2020 to 56.5% in March 2021; P < .01).
After applying a priori justified antibiotic use criteria, we found that the overall degree of empiric unjustified antibiotic use remained high for patients admitted with COVID-19 (36.5%-60.3%) and was largely driven by prescriptions from the ED. However, further analysis revealed a statistically significant decrease in empiric antibiotic LOT per patient during the study period from 3.0 days in October 2020 to 0.9 days in March 2021 (P < .01). In addition, there was a statistically significant change in the mean (SD) LOS, which decreased from 16.3 (17.8) days in October 2020 to 9.7 (13.0) days in March 2021 (P = .02).