Preoperative Insulin Intensification to Improve Day of Surgery Blood Glucose Control
Background: Guidelines offer varying recommendations for preoperative long-acting basal insulin dosing, despite mounting evidence of the advantages of maintaining perioperative glucose levels between 80 and 180 mg/dL.
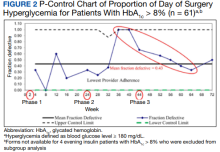
Observations: We iteratively adjusted health care practitioner (HCP) instructions to intensify insulin dosing on the evening before surgery for 195 consecutive patients with diabetes mellitus treated with long-acting basal insulin with an evening dosage. Baseline data was collected in phase 1. In phase 2, the preoperative insulin dose on the evening before surgery was increased for patients with hemoglobin A 1c (HbA 1c ) > 8%; in phase 3, it was increased for patients with HbA 1c ≤ 8% while sustaining the phase 2 change. Increased preoperative insulin doses did not change the rates of day of surgery (DOS) hyperglycemia or hypoglycemia. Overall, HCP adherence to the modified protocols was high (89%). A decline in HCP adherence after phase 2 protocol change was associated with a transient increase in DOS hyperglycemia. Patient adherence to preoperative medication instructions was high (86%) and was not affected by protocol changes.
Conclusions: Preoperative insulin intensification the evening before surgery did not change rates of DOS hyperglycemia or hypoglycemia. HCP adherence decreased transiently, which briefly increased DOS hyperglycemia rates in some patients.
A subgroup analysis of DOS glucose levels in insulin-treated patients with preoperative HbA1c levels > 8% did not demonstrate a change in the rate of
Only 7 of 424 (1.7%) patients with DM and 4 of 195 (2.1%) patients treated with evening, long-acting basal insulin had marked hyperglycemia (DOS glucose levels ≥ 300 mg/dL). Only 1 patient who was not on outpatient insulin treatment had surgery canceled for hyperglycemia.
Overall, 89% of the HCPs followed the preoperative insulin protocol. HCP adherence to the protocol decreased to 77% after the phase 2 change, often related to deviations from the protocol or when a prior version was used. By the end of phase 3, HCP adherence returned to the baseline rate (88%). Patient adherence to medication instructions was not affected by protocol changes (86% throughout the study period). Prospective data collection was briefly interrupted between January 18, 2019, and March 5, 2019, while designing our phase 2 intervention. We were unable to track the total number of eligible patients during this time, but were able to identify 8 insulin-treated patients with DM who underwent elective noncardiac surgery and included their data in phase 1.
Discussion
The management and prevention of immediate perioperative hyperglycemia and glycemic variability have attracted attention as evidence has mounted for their association with postoperative morbidity and mortality.1,2,17 Available guidelines for preventing DOS hyperglycemia vary in their recommendations for preoperative insulin management.7-10 Notably, concerns about iatrogenic hypoglycemia often hinder efforts to lower rates of DOS hyperglycemia.4 We successfully implemented an iterative intensification protocol for preoperative long-acting basal insulin doses on the evening before surgery but did not observe a lower rate of hyperglycemia. Importantly, we also did not observe a higher rate of hypoglycemia on the DOS, as observed in a previous study.5
The observational study by Demma and colleagues found that patients receiving 75% of their evening, long-acting basal insulin dose were significantly more likely to achieve target blood glucose levels of 100 to 180 mg/dL than patients receiving no insulin at all (78% vs 0%; P = .001). However, no significant difference was noted when this group was compared with patients receiving 50% of their evening, long-acting basal insulin doses (78% vs 70%; P = .56). This is more clinically pertinent as it is generally accepted that the evening, long-acting insulin dose should not be entirely withheld on the evening before surgery.5