Screening High-Risk Women Veterans for Breast Cancer
Background: Within the US Department of Veterans Affairs (VA), breast cancer prevalence has more than tripled from 1995 to 2012. Women veterans may be at an increased breast cancer risk based on service-related exposures and posttraumatic stress disorder (PTSD).
Methods: Women veterans aged ≥ 35 years with no personal history of breast cancer were enrolled at 2 urban VA medical centers. We surveyed women veterans for 5-year and lifetime risks of invasive breast cancer using the Gail Breast Cancer Risk Assessment Tool (BCRAT). Data regarding demographics, PTSD status, eligibility for chemoprevention, and genetic counseling were also collected. Descriptive statistics were used to determine results.
Results: A total of 99 women veterans participated, of which 60% were Black. In total, 35% were high risk with a 5-year BCRAT > 1.66%. Breast biopsies had been performed in 22% of our entire population; 57% had a family history positive for breast cancer. Comparatively, in our high-risk Black population, 33% had breast biopsies and 94% had a family history. High-risk patients were referred for chemoprevention; 5 accepted and 13 were referred for genetic counseling. PTSD was present in 31% of the high-risk subgroup.
Conclusions: A high percentage of Black patients participated in this pilot study, which also showed an above average rate of PTSD among women veterans who are at high risk for developing breast cancer. Historically, breast cancer rates among Black women are lower than those found in the general population. High participation among Black women veterans in this pilot study uncovered the potential for further study of this population, which is otherwise underrepresented in research. Limitations included a small sample size, exclusively urban population, and self-selection for screening. Future directions include the evaluation of genetic and molecular mutations in high risk Black women veterans, possibly even a role for PTSD epigenetic changes.
Methods
A high-risk breast cancer screening questionnaire based on the Gail BCRAT and including lifestyle questions was developed and included as a note template in the VA EMR. The James J. Peters VA Medical Center, Bronx, NY (JJPVAMC) and the Washington DC VA Medical Center (DCVAMC) ran a pilot study between 2015 and 2018 using this breast cancer screening questionnaire to collect data from women veterans. Quality Executive Committee and institutional review board approvals were granted respectively.
Eligibility criteria included women aged ≥ 35 years with no personal history of breast cancer. Most patients were self-referred, but participants also were recruited during VA Breast Cancer Awareness month events, health fairs, or at informational tables in the hospital lobbies. After completing the 20 multiple choice questionnaire with a study team member, either in person or over the phone, a 5-year and lifetime risk of invasive breast cancer was calculated using the Gail BCRAT. A woman is considered high risk and eligible for chemoprevention if her 5-year risk is > 1.66% or her lifetime risk is ≥ 20%. Eligibility for genetic counseling is based on the Breast Cancer Referral Screening Tool, which includes a personal or family history of breast or ovarian cancer and Jewish ancestry.
All patients were notified of their average or high risk status by a clinician. Those who were deemed to be average risk received a follow-up letter in the mail with instructions (eg, to follow-up with a yearly mammogram). Those who were deemed to be high risk for developing breast cancer were asked to come in for an appointment with the study principal investigator (a VA oncologist/breast cancer specialist) to discuss prevention options, further screening, or referrals to genetic counseling. Depending on a patient’s other health factors, a woman at high risk for developing breast cancer also may be a candidate for chemoprevention with tamoxifen, raloxifene, exemestane, anastrozole, or letrozole.
Data on the participant’s lifestyle, including exercise, diet, and smoking, were evaluated to determine whether these factors had an impact on risk status.
Results
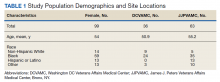
The JJP and DC VAMCs screened 103 women veterans between 2015 and 2018. Four patients were excluded for nonveteran (spousal) status, leaving 99 women veterans with a mean age of 54 years. The most common self-reported races were Black (60%), non-Hispanic White (14%), and Hispanic or Latino (13%) (Table 1).
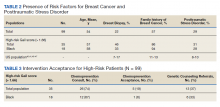
Women veterans in our study were nearly 3-times more likely than the general population were to receive a high-risk Gail Score/BCRAT (35% vs 13%, respectively).50,51 Of this subset, 46% had breast biopsies, and 86% had a positive family history. Thirty-one percent of Black women in our study were high risk, while nationally, 8.2 to 13.3% of Black women aged 50 to 59 years are considered high risk.50,51 Of the Black high-risk group with a high Gail/BCRAT score, 94% had a positive family history, and 33% had a history of breast biopsy (Table 2).
Of the 35 high-risk patients 26 (74%) patients accepted consultations for chemoprevention and 5 (19%) started chemoprevention. Of this high-risk group, 13 (37%) patients were referred for genetic counseling (Table 3).44 The prevalence of PTSD was present in 31% of high-risk women and 29% of the cohort (Figure).The lifestyle questions indicated that, among all participants, 79% had an overweight or obese body mass index; 58% exercised weekly; 51% consumed alcohol; 14% were smokers; and 21% consumed 3 to 4 servings of fruits/vegetables daily.