Retrospective Review on the Safety and Efficacy of Direct Oral Anticoagulants Compared With Warfarin in Patients With Cirrhosis
Purpose: Patients with cirrhosis needing anticoagulation therapy have historically been prescribed warfarin. New retrospective research has concluded that in patients with cirrhosis direct oral anticoagulants (DOACs) have similar or lower bleeding rates compared with that of warfarin. This study compares the safety and efficacy of DOACs with that of warfarin in patients with cirrhosis.
Methods: A retrospective chart review was conducted in adult patients with cirrhosis taking either apixaban, dabigatran, edoxaban, rivaroxaban, or warfarin. Exclusion criteria consisted of patients prescribed triple antithrombotic therapy (dual antiplatelet therapy plus an anticoagulant) and indications other than nonvalvular atrial fibrillation (NVAF) and venous thromboembolism (VTE). The primary endpoint was all-cause bleeding, and the secondary endpoints were failed efficacy and major bleeding as defined by the International Society on Thrombosis and Haemostasis in 2005. Failed efficacy was a combination endpoint including the development of VTE, stroke, myocardial infarction and/or death. Patient data were collected from the Computerized Patient Record System from October 31, 2014 to October 31, 2018.
Results: The study included 42 patients in the DOAC group and 37 patients in the warfarin group. Baseline characteristics were not significantly different between groups except for the Child-Turcotte-Pugh score, Model for End-Stage Liver Disease score, international normalized ratio, and number of days on anticoagulation therapy. The rate of all-cause bleeding in the DOAC group was 16.7% (n = 7) vs 21.6% (n = 8) in the warfarin group ( P = .7). The rate of major bleeding in the DOAC group was 2.4% (n = 1) vs 5.4% (n = 2) in the warfarin group ( P = .6). The rate of failed efficacy in the DOAC group was 7.1% (n = 3) compared with 8.1% (n = 3) in the warfarin group ( P = .9). Subgroup analysis of all-cause bleeding did not identify any significant trends between groups.
Conclusions: There were no statistically significant differences identified between the rates of all-cause bleeding, major bleeding, and failed efficacy between the DOACs and warfarin groups. DOACs may be a safe alternative to warfarin in patients with cirrhosis requiring anticoagulation for NVAF or VTE, but large randomized trials are required to confirm these results.
Efficacy Outcomes
There were 3 events in the DOAC group and 3 events in the warfarin group (P = .99). In the DOAC group, 2 patients experienced a pulmonary embolism, and 1 patient experienced a MI. In the warfarin group, 3 patients died (end-stage heart failure, unknown cause due to death at an outside hospital, and sepsis/organ failure). There were no statistically significant differences between the composite endpoint of failed efficacy or the individual endpoints of VTE, stroke, MI, and death.
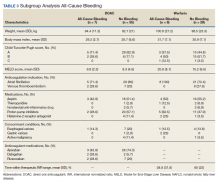
Subgroup Analysis
A prespecified subgroup analysis was conducted to determine risk factors for all-cause bleeding within each treatment group (Table 3). No significant trends were observed in the following risk factors: Child-Turcotte-Pugh score, indication for anticoagulation, use of NSAIDs, PPIs or H2RAs, presence of gastric or esophageal varices, active malignancies, and time within therapeutic INR range in the warfarin group. Patients with bleeding events had slightly increased weight and BMI vs patients without bleeding events. Within the warfarin group, patients with bleeding events had slightly elevated MELD scores compared to patients without bleeding events. There was an equal balance of patients prescribed aspirin therapy between the groups with and without bleeding events. Overall, no significant risk factors were identified for all-cause bleeding.
Discussion
Initially, patients with cirrhosis were excluded from DOAC trials due to concerns for increased bleeding risk with hepatically eliminated medications. New retrospective research has concluded that in patients with cirrhosis, DOACs have similar or lower bleeding rates when compared directly to warfarin.9,10
In this study, no statistically significant differences were detected between the primary and secondary outcomes of all-cause bleeding, major bleeding, or failed efficacy. Subgroup analysis did not identify any significant risk factors with respect to all-cause bleeding among patients in the DOAC and warfarin groups. To meet 80% power, 212 patients needed to be enrolled in the study; however, only 79 patients were enrolled, and power was not met. The results of this study should be interpreted cautiously as hypothesis-generating due to the small sample size. Strengths of this study include similar baseline characteristics between the DOAC and warfarin groups, 4-year length of retrospective data review, and availability of both inpatient and outpatient EHR limiting the amount of missing data points.
Baseline characteristics were similar between the groups except for mean INR, Child-Turcotte-Pugh score, MELD score, and number of days on anticoagulation therapy. The difference in mean INR between groups is expected as patients in the warfarin group have a goal INR of 2 to 3 to maintain therapeutic efficacy and safety. INR is not used as a marker of efficacy or safety with DOACs; therefore, a consistent elevation in INR is not expected. Child- Turcotte-Pugh scores are calculated using INR levels.11 When calculating the score, patients with an INR < 1.7 receive 1 point; patients with an INR between 1.7 and 2.3 receive 2 points.11 Therefore, patients in the warfarin group will have artificially inflated Child-Turcotte-Pugh scores as this group has goal INR levels of 2 to 3. This makes Child-Turcotte-Pugh scores unreliable markers of disease severity in patients using warfarin therapy. When the INR scores for patients prescribed warfarin were replaced with values < 1.7, the statistical difference disappeared between the warfarin and DOAC groups. The same effect is seen on MELD scores for patients prescribed warfarin therapy. The MELD score is calculated using INR levels.12 MELD scores also will be artificially elevated in patients prescribed warfarin therapy due to the INR elevation to between 2 and 3. When MELD scores for patients prescribed warfarin were replaced with values similar to those in the DOAC group, the statistical difference disappeared between the warfarin and DOAC groups.
The last statistically significant difference was found in number of days on anticoagulant therapy. This difference was expected as warfarin is the standard of care for anticoagulation treatment in patients with cirrhosis. The first DOAC, dabigatran, was not approved by the US Food and Drug Administration until 2010.13 DOACs have only recently been used in patients with cirrhosis accounting for the statistically significant difference in days on anticoagulation therapy between the warfarin and DOAC groups.