Retrospective Review on the Safety and Efficacy of Direct Oral Anticoagulants Compared With Warfarin in Patients With Cirrhosis
Purpose: Patients with cirrhosis needing anticoagulation therapy have historically been prescribed warfarin. New retrospective research has concluded that in patients with cirrhosis direct oral anticoagulants (DOACs) have similar or lower bleeding rates compared with that of warfarin. This study compares the safety and efficacy of DOACs with that of warfarin in patients with cirrhosis.
Methods: A retrospective chart review was conducted in adult patients with cirrhosis taking either apixaban, dabigatran, edoxaban, rivaroxaban, or warfarin. Exclusion criteria consisted of patients prescribed triple antithrombotic therapy (dual antiplatelet therapy plus an anticoagulant) and indications other than nonvalvular atrial fibrillation (NVAF) and venous thromboembolism (VTE). The primary endpoint was all-cause bleeding, and the secondary endpoints were failed efficacy and major bleeding as defined by the International Society on Thrombosis and Haemostasis in 2005. Failed efficacy was a combination endpoint including the development of VTE, stroke, myocardial infarction and/or death. Patient data were collected from the Computerized Patient Record System from October 31, 2014 to October 31, 2018.
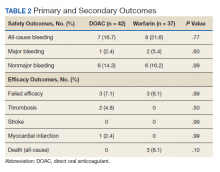
Results: The study included 42 patients in the DOAC group and 37 patients in the warfarin group. Baseline characteristics were not significantly different between groups except for the Child-Turcotte-Pugh score, Model for End-Stage Liver Disease score, international normalized ratio, and number of days on anticoagulation therapy. The rate of all-cause bleeding in the DOAC group was 16.7% (n = 7) vs 21.6% (n = 8) in the warfarin group ( P = .7). The rate of major bleeding in the DOAC group was 2.4% (n = 1) vs 5.4% (n = 2) in the warfarin group ( P = .6). The rate of failed efficacy in the DOAC group was 7.1% (n = 3) compared with 8.1% (n = 3) in the warfarin group ( P = .9). Subgroup analysis of all-cause bleeding did not identify any significant trends between groups.
Conclusions: There were no statistically significant differences identified between the rates of all-cause bleeding, major bleeding, and failed efficacy between the DOACs and warfarin groups. DOACs may be a safe alternative to warfarin in patients with cirrhosis requiring anticoagulation for NVAF or VTE, but large randomized trials are required to confirm these results.
Statistical Analysis
Data were analyzed using descriptive and inferential statistics. Continuous data were analyzed using the Student t test, and categorical data were analyzed using the Fisher exact test. Previous studies determined an all-cause bleeding rate of 10 to 17% for warfarin compared with 5% for DOACs.7,8 To detect a 12% difference in the all-cause bleeding rate between DOACs and warfarin, 212 patients would be needed to achieve 80% power at an α level of 0.05.
Results
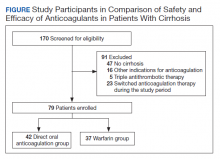
A total of 170 patients were screened, and after applying inclusion and exclusion criteria, 79 patients were enrolled in the study (Figure). The DOAC group included 42 patients, and the warfarin group included 37 patients. In the DOAC group, 69.1% (n = 29) of patients were taking apixaban, 21.4% (n = 9) rivaroxaban, and 9.5% (n = 4) dabigatran. There were no patients prescribed edoxaban during the study period.
Baseline characteristics were similar between the 2 groups except for Child-Turcotte-Pugh score, MELD score, mean INR, and number of days on anticoagulation therapy (Table 1). Most of the patients were male (98.7%), and the mean age was 71 years. The most common causes of cirrhosis were viral (29.1%), nonalcoholic fatty liver disease (NAFLD) (24.1%), multiple causes (22.8%), and alcohol (21.5%). Sixty-two patients (78.5%) had a NVAF indication for anticoagulation. The average CHA2DS2-VASc score was 3.7. Aspirin was prescribed in 51.9% (n = 41) of patients, and PPIs were prescribed in 48.1% (n = 38) of patients. At inclusion, esophageal varices were present in 13 patients and active malignancies were present in 6 patients.
Statistically significant differences in baseline characteristics were found between mean INR, Child-Turcotte-Pugh scores, MELD scores, and number of days on anticoagulant therapy. The mean INR was 1.3 in the DOAC group compared with 2.1 in the warfarin group (P = .0001). Eighty-one percent (n = 34) of patients in the DOAC group had a Child-Turcotte-Pugh score of A compared with 43.2% (n = 16) of patients in the warfarin group (P = .0009). Eight patients in the DOAC group had a Child-Turcotte-Pugh score of B compared with 19 patients in the warfarin group (P = .004). The mean MELD score was 9.4 in the DOAC group compared with 16.3 in the warfarin group (P = .0001). The mean days on anticoagulant therapy was 500.4 days for the DOAC group compared with 1,652.4 days for the warfarin group (P = .0001).
Safety Outcome
The primary outcome comparing all-cause bleeding rates between patients on DOACs compared with warfarin are listed in Table 2. With respect to the primary outcome, 7 (16.7%) patients on DOACs experienced a bleeding event compared with 8 (21.6%) patients on warfarin (P = .77). No statistically significant differences were detected between the DOAC and warfarin groups with respect to all-cause bleeding. Seven bleeding events occurred in the DOAC group; 1 met the qualification for major bleeding with a suspected gastrointestinal (GI) bleed.6 The other 6 bleeding episodes in the DOAC group consisted of hematoma, epistaxis, hematuria, and hematochezia. Eight bleeding events occurred in the warfarin group; 2 met the qualification for major bleeding with an intracranial hemorrhage and upper GI bleed.6 The other 6 bleeding episodes in the warfarin group consisted of epistaxis, bleeding gums, hematuria, and hematochezia. There were no statistically significant differences between the rates of major bleeding and nonmajor bleeding between the DOAC and warfarin groups.