Remote Temperature Monitoring of the Diabetic Foot: From Research to Practice
Introduction: Diabetic foot ulcers (DFUs) are devastating, common, and costly. The mortality of veterans following a DFU is sobering with ulceration recognized as a significant marker of disease severity. Given the dramatic impact of diabetic foot complications to the veteran and the US health care system, the US Department of Veterans Affairs (VA) has long recognized the importance of preventive care for those at risk. Telemedicine has been suggested as a modality to reach veterans at high risk of chronic wound formation.
Observations: The purpose of this review is to: (1) present the evidence supporting once-daily remote temperature monitoring (RTM), a telemedicine approach critical to improving both veteran access to care and diabetic foot outcomes; (2) summarize a 2017 study published by VA providers who have advanced clinical understanding of RTM; (3) present previously unpublished data from this study comparing high-risk VA and non-VA cohorts, highlighting the opportunity for additional focus on DFU prevention within the VA; and (4) report on recent VA use of a RTM technology based on this research, emphasizing lessons learned and best practices.
Conclusions: There is a significant opportunity to shift diabetic foot care from treatment to prevention, improving veteran outcomes and reducing resource utilization. RTM is an evidence-based, recommended, but underused telemedicine solution that can catalyze this needed paradigm shift.
Clinical Best Practices
Treating preulcerative lesions urgently and aggressively. Callus and other preulcerative lesions often cause progressive tissue damage and poor outcomes. When identified, these lesions should be promptly treated to ensure best outcomes.24
Recognizing the limits of patient self-examinations. Comorbidities such as visual impairment and reduced joint mobility often preclude patients from completing rigorous self-examinations of the foot, which is especially critical while collecting subjective history from the patient during triage of inflammation. A caregiver or spouse can help inspect the foot during outreach and provide additional context.36
Interpreting a benign foot on examination. Because RTM has been demonstrated to detect inflammation preceding a foot ulcer as many as 5 weeks before presentation to the clinic, some veterans may have few signs or symptoms of acute risk during examination. Often, the damage is to subcutaneous tissue resulting from repetitive microtrauma. Research suggests that clinical examination in these cases is often unreliable for identifying the earliest signs of risk, such as palpation to identify subtle temperature changes secondary to inflammation.37 If a patient has refractory inflammation requiring examination and presents with an otherwise unremarkable foot, it is an opportunity to evaluate whether the patient’s shoewear remains appropriate or has worn out, to communicate the veteran’s ongoing elevated risk, and to educate on the importance of diligence in daily foot self-examinations, daily use of the foot temperature monitoring, and continued off-loading until the inflammation resolves.
Communicating the distinction between healing and remission. Although healing is the goal of wound care, patients should be educated that the underlying disease remains after epithelialization. In some cases, tissue deep to the skin has not completed remodeling, and the patient is at acute risk of recurrence. Remission is a powerful metaphor that better describes the patient’s ongoing risk to encourage continued healthy routines and diligent self-care.38Considering the entirety of both feet for recurrence. Critical risk factors for diabetic foot complications, such as peripheral neuropathy and PAD, exist in both limbs, and patients with a history of wounds often develop new complications to different ipsilateral locations, or in as many as 48% of cases, to the contralateral foot.35 For best outcomes, detected inflammation should be treated aggressively independent of whether the location coincides with an area of previous concern.
Encouraging adherence, routine, and empowerment. Advanced diabetes mellitus and neuropathy may impact a patient’s executive function, and multiple studies have reported that patients at risk for inflammatory foot diseases exhibit fatalism toward their foot care and outcomes.39-41 Consistent education, encouragement, empowerment, and establishment of positive routines are needed to ensure high adherence with all preventive care regimens, including RTM.
Case Presentations
The following case series illustrates many of these clinical best practices and characterizes the potential benefits of RTM to veterans within the VA.
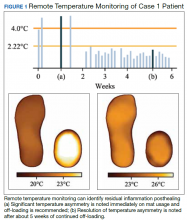
Case 1: Prevention After Healing
A veteran underwent a Chopart amputation and was recommended to use the mat after healing was perceived. Immediately on use of the study mat, the patient was found to have inflammation to the surgical incision (Figure 1). Clinical staff was alerted to the findings, and the patient was instructed to limit further walking and continue off-loading in his removable cast walker, per protocol. The inflammation of the operative foot quickly reduced, and the patient continued healing successfully, potentially avoiding incisional dehiscence and possible postoperative infection.