Remote Temperature Monitoring of the Diabetic Foot: From Research to Practice
Introduction: Diabetic foot ulcers (DFUs) are devastating, common, and costly. The mortality of veterans following a DFU is sobering with ulceration recognized as a significant marker of disease severity. Given the dramatic impact of diabetic foot complications to the veteran and the US health care system, the US Department of Veterans Affairs (VA) has long recognized the importance of preventive care for those at risk. Telemedicine has been suggested as a modality to reach veterans at high risk of chronic wound formation.
Observations: The purpose of this review is to: (1) present the evidence supporting once-daily remote temperature monitoring (RTM), a telemedicine approach critical to improving both veteran access to care and diabetic foot outcomes; (2) summarize a 2017 study published by VA providers who have advanced clinical understanding of RTM; (3) present previously unpublished data from this study comparing high-risk VA and non-VA cohorts, highlighting the opportunity for additional focus on DFU prevention within the VA; and (4) report on recent VA use of a RTM technology based on this research, emphasizing lessons learned and best practices.
Conclusions: There is a significant opportunity to shift diabetic foot care from treatment to prevention, improving veteran outcomes and reducing resource utilization. RTM is an evidence-based, recommended, but underused telemedicine solution that can catalyze this needed paradigm shift.
New Research
The data collected during this study has led to new research and advancements in RTM. A recent publication by Gordon and colleagues investigated whether RTM is less accurate in cohorts with perceived challenges.33 They include patients with recently healed wounds and those with a history of partial foot amputation. There was no difference in the accuracy or lead time for either cohort relative to the entire cohort, suggesting that RTM is appropriate for monitoring patients with recently healed DFUs or partial foot amputations.
In another recent study, the data were used to derive a novel approach to monitor a single at-risk foot.34 The practice of RTM has traditionally required comparing temperatures between contralaterally matched plantar locations on the feet, thus limiting its use in patients with a history of major lower extremity amputation and patients being treated for a wound, which may be bandaged or in an off-loading cast or boot. Because the risk factors for DFUs exist in both limbs, these patients are at high risk for developing complications to the contralateral foot and may benefit from preventive once-daily foot temperature monitoring. The investigators empirically derived a novel monitoring approach for patients without a contralateral control. This approach was found to predict 91% of impending plantar DFUs on average 41 days before clinical presentation with a false positive rate of 54%.
Additional Focus on Prevention
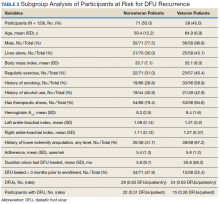
Table 2 shows previously unpublished data from a subgroup analysis between veteran and nonveteran participants in the study.25 These descriptive statistics reinforce some widely held assumptions regarding the high-risk veteran population and challenge others. For example, compared with the nonveteran participants, the veteran cohort unsurprisingly had a larger ratio of male participants (P < .01), had a higher rate of cigarette use (P < .01), and was more likely to live alone (although not at a statistically significant level). Veterans in the study had body mass index, rates of alcohol use, frequency of exercise, and glucose control comparable to that of nonveterans.
The potential impact of the PAVE program is clear in several of these comparisons. Although as few as 15% of patients use therapeutic shoes routinely, PAVE ensures that the majority of veterans receive them. Nearly 95% of veterans have therapeutic shoes compared with about 80% of nonveteran participants (P < .05). Veterans also had higher ankle-brachial index results (P < .05), although on average both cohorts were within normal clinical parameters. Veterans had a significantly longer duration since healing from the most recent wound, and fewer veteran participants had a wound that healed in the 3 months prior to the study. Despite this, during the study veterans had annualized DFU incidence equal to that of nonveterans. Furthermore, veterans also had significantly higher rates of amputation prior to participation. That these critical outcomes for veterans are no better than those observed in other care environments despite PAVE suggests that approaches recommended via PAVE alone are insufficient to significantly arrest DFU recurrence, and even more focus on prevention in the VA may be warranted.