Using Stroke Order Sets to Improve Compliance With Quality Measures for Ischemic Stroke Admissions
Results
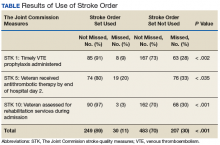
Of 323 admitted patients with stroke, 93 admissions were entered using the stroke order set. Out of these completed orders, 85 (91%) veterans admitted for ischemic stroke or TIA management received timely VTE prophylaxis, and 8 (9%) veterans did not. Of the 230 admissions completed without using the stroke order set, 167 (73%) veterans received timely VTE prophylaxis, and 63 (28%) veterans did not. Additionally out of the 93 veterans admitted using the stroke order set, 74 (80%) veterans admitted for the management of ischemic stroke received antithrombotic therapy by end of hospital day 2, whereas 19 (20%) veterans did not, and there were no clear contraindications documented as to why.
For veterans admitted without using the order set, 167 (73%) veterans admitted for the management of ischemic stroke received antithrombotic therapy by the end of hospital day 2, whereas 76 (33%) veterans did not. Last, 90 (97%) of the 93 veterans admitted for stroke workup using the order set were assessed for rehabilitation services during admission, whereas 3 (3%) were not. For the veterans who were admitted without using the stroke order set, 162 (70%) were assessed for rehabilitation services during admission, whereas 68 (30%) were not.
Out of 969 compliance measures looked at, 237 measures were missed and 732 measures were appropriately completed irrespective of whether the stroke order set was used. Out of the 279 admissions where the stroke order set was used, 249 (89%) quality measures were met.
The study threshold for meeting the standards was the national average for 2015, which was 91.1% for the administration of VTE prophylaxis in a timely manner, 97.9% for administering antithrombotic therapy by end of hospital day 2, and 94.2% for assessment of the patient by rehabilitation services during the admission.
Discussion
Despite the repeated training and orientation, compliance to the order set usage was not optimal, likely secondary to a frequent change in the pool of admitting physicians using the order set. Also, the order set was new to staff, thus, admitting physicians sometimes forgot to use them. The next step in this project will be to create an order set for the ED with markers for tracing usage. These order sets will include all quality measures that need to be completed in the ED, such as the NIH Stroke Scale timely documentation, tPA administration data, swallow screen prior to po intake, and stroke transfers.
This QI project also streamlined the process for stroke admissions. With the creation of the order set, all orders needed for stroke were available to the admitting physician, resulting in less need for searching the order individually from a large pool of orders (Figures 3 and 4).
Several reputable institutions have quality metrics and performance measures typically focused on processes of care based on specific clinical guidelines recommendations. Clinical guidelines are usually based on sufficient evidence that failure to provide the recommended care is likely to result in suboptimal clinical outcomes. Stroke quality measure compliance is part of the Reporting Hospital Quality Data for Annual Payment Update (RHQDAPU) initiative, and most hospitals will be required to report these measures in order to receive full Medicare payments.11