Using Stroke Order Sets to Improve Compliance With Quality Measures for Ischemic Stroke Admissions
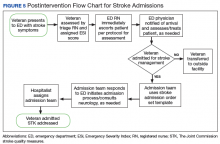
The hospitalist created evidence-based admission orders for all patients admitted for stroke or transient ischemic attack (TIA).The measures used were from the JC Specification Manual for Joint Commission National Quality as well as The American College of Cardiology/American Heart Association classification of care metrics.5
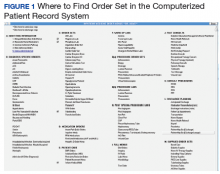
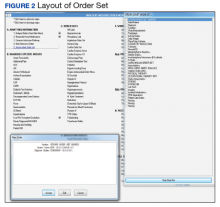
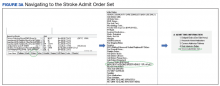
The order sets were reviewed and confirmed by a neurologist. The JC quality measures required for the care of patients admitted for stroke management were embedded in these order sets. These order sets were placed directly under the general admission orders in the Computerized Patient Record System (CPRS)
The quality measures included:
- STK 1: Veteran admitted for stroke received venous thromboembolic (VTE) prophylaxis in a timely manner. Pharmacologic management for VTE prophylaxis with subcutaneous low-molecular weight heparin and/or application of bilateral sequential compression devices were tracked.
- STK 5: Veteran admitted for stroke administered antithrombotic therapy by end of hospital day 2. Aspirin, aspirin/dipyridamole, and ticlopidine were tracked.
- STK 10: Veteran admitted for stroke assessed for rehabilitation services during admission. Physical therapy and occupational therapy consult placements were tracked. Quality measures, such as administration of tissue plasminogen activator (tPA), were not embedded in the order set because veterans who met the criteria for tPA were immediately administered tPA in the ED or transferred to the closest stroke center.
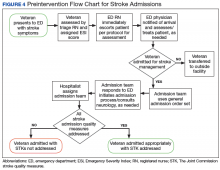
In this QI project, only quality measures that had to be completed in the inpatient setting were included. Quality measures such as tPA administration, National Institutes of Health (NIH) Stroke Scale timely documentation, swallow screen prior to po intake, and stroke transfers were completed in the ED prior to clearance for admission, so these were not included in the project. The Atlanta VAMC ED has protocols to care for these patients, but they do not have order sets with markers that could trace their usage.
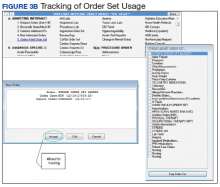
All admission orders placed were reviewed by a QI team to check whether the stroke order set had been used. The ability to determine order set use was accomplished by adding the unique identifier Stroke Order Set Marker, which allowed for querying using structured query language (SQL) within the Corporate Data Warehouse.
Next, all admissions were checked through chart review for compliance with quality measures. Admissions that had not been completed for all quality measures were identified, and the physicians or NPs caring for those veterans were alerted. These order sets were supposed to be used during admission of all patients admitted for stroke management or workup; however, some patients were admitted without the use of the order sets.
The successful completion of the quality measures were then compared between the groups of patients admitted using the order set and the group of patients in which the order set was not used at their admission. The physicians were provided acceptable reasons, including contraindications to certain medications such as patient history of allergy. The admitting physician made decisions on the antiplatelet medications to use or on neurology recommendations. The neurology department was consulted on all patients who had acute or subacute ischemic stroke findings on magnetic resonance imaging (MRI).
At the beginning of the month, internal medicine residents from Emory University and Morehouse School of Medicine received orientation on the use of the stroke order set from the team NP and chief resident. Tips on how to use the CPRS and how to access the stroke order sets also were created.
One challenge the project faced was the continuous change in the admitting team pool: Some residents did not remember to use the stroke order sets.