Aggressive Crystalloid Resuscitation Ups Morbidity
Major Finding: Patients with a crystalloid to packed red blood cell ratio of more than 1.5:1 had a significant, more than twofold higher independent risk of multiple organ failure and acute respiratory distress and nearly a fourfold higher risk of abdominal compartment syndrome.
Data Source: Secondary analysis of a prospective cohort of 452 blunt trauma patients.
Disclosures: Dr. Neal disclosed a Glue Grant from the Inflammation and the Host Response to Injury research program. Dr. Kerby reported no conflicts of interest.
NAPLES, FLA. - A rising crystalloid-to–packed red blood cell ratio increases the risk of morbidity in patients requiring massive transfusion, with high ratios of more than 1.5:1 showing the most dramatic increase in risk.
The finding is based on a secondary analysis of 452 blunt trauma patients who were transfused with a median of 17 L of crystalloid (C) resuscitation and a median of 16 units of packed red blood cells (PRBC) within the first 24 hours of admission. Overall mortality and multiple organ failure rates for the multicenter prospective cohort were 21% and 65%, respectively. Their median Injury Severity Score (ISS) was 34.
The secondary analysis divided the cohort at its median C:PRBC ratio, with 225 patients defined as having a high C:PRBC ratio and 227 patients as having a low C:PRBC ratio.
Logistic regression analysis revealed that the 24-hour C:PRBC ratio was significantly associated with a greater independent risk of multiple organ failure (MOF), acute respiratory distress syndrome (ARDS), and abdominal compartment syndrome (ACS). There was no significant association with mortality or nosocomial infection. Dr. Matthew D. Neal, a general surgery resident at the University of Pittsburgh, presented the study results at the annual meeting of the Eastern Association for the Surgery of Trauma.
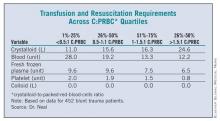
The researchers then conducted a dose-response analysis, dividing the cohort into four quartiles based on C:PRBC ratios. (See box below.) Interestingly, patients in the highest quartile (those with a C:PRBC ratio greater than 1.5:1) received by far the most crystalloid and the least amount of blood and blood products, said Dr. Neal. They also had a significant, more-than-twofold-higher independent risk of MOF (odds ratio, 2.6) and ARDS (OR, 2.5) and a nearly a fourfold higher risk of ACS (OR, 3.6).
Appropriate ratios of blood and blood products in massive transfusion protocols have been the focus of much research, but crystalloid has yet to be studied in a ratio-based manner, despite its being a mainstay of resuscitation since the 1950s, Dr. Neal said. There are recommendations in the hemostatic resuscitation literature to minimize its use because of the cellular and inflammatory disturbances associated with crystalloid infusion in the setting of trauma and hemorrhagic shock, but no specific guidelines exist.
Crystalloid use decreased over the study period of 2003-2008, according to an additional analysis that divided the cohort at its median into early and late time points. The mean total volume of crystalloid administered was significantly lower in the late group (12 L) than in the early group (16 L), Dr. Neal said. Patients treated with the high volumes of crystalloid for early resuscitation had a dramatically increased risk of ARDS and ACS – but not MOF – despite having lower ISS scores.
"Further high-level research is needed to see if crystalloid-to–packed red blood cell ratio should be incorporated into massive transfusion protocols," he said.
Invited discussant Dr. Jeffrey Kerby of the University of Alabama at Birmingham said that the analysis is based on the assumption that resuscitation ratios are fixed and stable; yet, in fact, they are dynamic and can change from hour to hour. Thus, patients could shift back and forth between C:PRBC groups, which could have a significant impact on outcomes. By excluding patients who died within the first 24 hours, he added, the analysis could have excluded a large number of patients and the genuine possibility of the findings.
Nonetheless, Dr. Kerby said he enjoyed the paper and asked what fluid the authors would recommend for use during the initial 24 hours.
Dr. Neal responded, "I think that we’re all still stuck with crystalloid for better or for worse until something better emerges, but I think our new literature is guiding us as to what the right outcomes are to measure – intravascular depletion and hypotension."
Dr. Neal’s paper won the 2011 Raymond H. Alexander, M.D., Resident Paper Competition of the EAST Foundation.
Dr. Neal disclosed a Glue Grant from the Inflammation and the Host Response to Injury research program. Dr. Kerby reported no conflicts of interest.