How patients benefit when you add an HPV test to screening for cervical Ca
Together, a previous abnormal Pap test, infrequent screening, and a current positive HPV test warrant special handling of this patient’s case
IN THIS ARTICLE
Likely questions
Because HPV testing plays an ever-increasing role in cervical screening, it presents a new set of educational challenges.6 Until recently, clinicians generally avoided discussing the cause of abnormal cervical cytology, CIN, and cervical cancer. However, when a woman is tested for high-risk HPV along with the Pap test in primary screening, the subject can no longer be skirted. Already the HPV vaccine and widespread use of the Web by patients have changed the information base on HPV. Education can begin at the time of the Pap and HPV tests, need not be extensive, and often can deflect undue anxiety and many of the patient’s questions about a positive result.
G.A. has been married for nearly 22 years. Her husband has been her only partner, but he was sexually active before they were married. She is naturally concerned about how long she has had HPV and what this means for her relationship. Her questions are universal: How and when did I become infected? What is my risk and that of my partner? How will I be managed? Will I always have HPV?
These questions may seem daunting, but the answers can be kept simple and short and still provide enough information to be reassuring and to prepare the patient for a possible positive test result.
Quantify risk before you select management
Most women with normal cytology but a first-time positive HPV test do not have CIN 2,3 or greater.11-14 A National Cancer Institute prospective 10-year follow-up of more than 20,000 women screened at enrollment with both the HPV test and cytology demonstrated that only 4.4% of the HPV-positive, Pap-negative women had CIN 3 or cancer detected over the following 3 to 5 years, and only 7% did by 10 years.13,14 These rates are similar to those found in other studies and are about half the risk represented by a Pap result of atypical squamous cells of undetermined significance (ASC-US).15
Therefore, because of the low immediate risk for high-grade cervical neoplasia and the extremely rare occurrence of cervical cancer in this setting, immediate referral to colposcopy is not recommended in routine cases (FIGURE 1).9,15 Instead, repeating Pap and HPV testing in 6 to 12 months yields a more accurate picture of risk by determining whether the HPV is only transient or is persistent. Only persistent HPV is associated with significant risk for CIN 2,3. Therefore, repeating the tests, rather than sending the patient to immediate colposcopy, allows the 45% to 70% of HPV infections destined to be transient to resolve spontaneously, but will still detect most significant lesions within a reasonable period of time.15
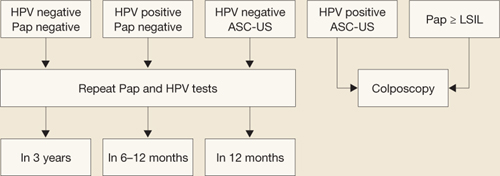
FIGURE 1 How to interpret the HPV test and cytology combined: NCI–ASCCP Interim Guidance
SOURCE: National Cancer Institute and the American Society for Colposcopy and Cervical Pathology. Adapted from Wright et al15
ASC-US=atypical squamous cells of undetermined significance; HPV=human papillomavirus; LSIL=low-grade squamous intraepithelial lesions.If G.A. is managed in this way and, at the 6- and 12-month repeats of both tests, has a positive HPV test (regardless of the cytology finding) or any abnormal Pap test result other than HPV-negative/ASC-US, she should undergo colposcopy.15 A test designated as HPV-negative/ASC-US can be managed by repeat testing in 12 months.
Remember: Even though a repeat positive HPV test increases the patient’s risk of CIN 2,3 significantly, it is specifically not recommended to treat the cervix solely on the basis of a persistently positive HPV test without evidence of CIN or cervical cancer.
This patient warrants a different approach—here’s why
Although repeat Pap and HPV testing in 6 to 12 months is the standard recommendation for women with a normal Pap test and positive HPV results, extenuating circumstances may exist. Clinical judgment always trumps routine recommendations in these cases.
The progression of CIN 3 to cervical cancer is usually a slow process that occurs over many years.6 Therefore, delaying colposcopy for 6 to 12 months will probably not increase risk significantly even if a high-grade lesion is already present. But G.A.’s case involves a number of variables that may increase her risk enough to justify immediate colposcopy:
- an abnormal Pap test more than 20 years ago
- a history of irregular screening
- no screening within the past 5 years until the current testing
- concern that her last Pap result was either minimally abnormal or of limited quality.
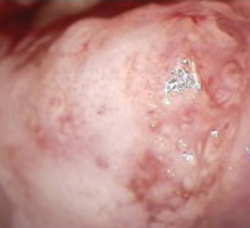
Lack of access to any earlier records further limits the physician’s ability to adequately judge G.A.’s risk. Because of these concerns, the physician asks G.A. to come in for colposcopy, at which time a 2-quadrant CIN 3 lesion is found (FIGURE 2). The patient is treated by loop electrosurgical excision procedure and has normal cytology and a negative HPV test result on follow-up.