Sexual dysfunction: The challenge of treatment
Identifying “blocks” in the sexual response cycle helps reveal the cause, and using a medical model points to optimal management.
Testosterone levels have little correlation with sexual desire in cycling women or women on oral contraceptives.3 Most studies have found no correlation between testosterone levels and sexual function in perimenopausal or naturally menopausal women.4,5 Other studies have failed to show a difference in testosterone levels between women with arousal disorders and normal controls.6
Testosterone therapy may be effective in surgically menopausal women with low libido. Shifrin and colleagues7 randomized 75 surgically menopausal women being treated with conjugated equine estrogens to placebo or transdermal testosterone, 150 or 300 μg per day, in a crossover trial. They reported, “Despite an appreciable placebo response, the higher testosterone dose resulted in further increases in scores for frequency of sexual activity and pleasure-orgasm. At the higher dose, the percentages of women who had sexual fantasies, masturbated, or engaged in sexual intercourse at least once a week increased 2 to 3 times from base line.”
Testosterone is not yet approved for female sexual dysfunction, but a transdermal testosterone is being proposed for women with hypoactive sexual desire disorder who have had bilateral oophorectomy.
Excitement phase disorders
These disorders are caused by pain with intercourse. What the patient says about the site of pain and when she began experiencing pain help form the differential diagnosis.
Dyspareunia can be due to physiological causes such as obstetric laceration, endometriosis, pelvic inflammatory disease, vaginitis, vulvar disease, and vestibulitis. Interstitial cystitis and inflammatory bowel disease can cause dyspareunia, as can a simple fungal infection. Ask how long the pain continues after intercourse. If internal pain continues for hours, it is highly suggestive of intra-abdominal pathology.
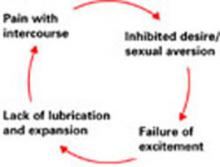
Any cause of pain can begin a self-perpetuating conditioned response cycle that leads to inhibited desire. Anything that causes pain elicits aversion behavior, even without the stimulus. With conditioned response comes failure of excitement, which is where the sexual response cycle is interrupted.
When pain interrupts the sexual response cycle, the patient may still have intercourse, but without excitement, lubrication, and vaginal expansion—and with consequent further pain. Further attempts at intercourse then cause more pain, leading to the cycle of dyspareunia. Pain may be introital, vaginal, or deep. The pain may be reproduced on exam.
Treatment is twofold. Identify and correct source of pain first. Then the patient must learn that intercourse is not painful but pleasurable. Sensate focus exercises are often useful.
Vaginismus, an involuntary spasm of muscles around the outer third of the vagina, may make penetration impossible. Vaginismus can be caused by pain, severe negative parental attitudes about sex, or extreme religious orthodoxy. These patients may be hyper-feminine. They often have bizarre mental images of their genitals. They usually have a partner who supports the dysfunction.
Treatment involves dilators, but the purpose is not to dilate the vagina. It is to learn to have something in the vagina and to confront fears and feelings rregarding penetration. Treatment must involve the partner.
Plateau and orgasmic dysfunctions
Delayed or absent orgasm is common. It may be primary or secondary, global, situational, or random. Etiologies include performance anxiety, fear of loss of control, and boredom. Patients with orgasmic dysfunction often develop “spectator” behavior. When they reach plateau they begin to wonder if they will have orgasm. They begin to watch to see what is happening rather than participating. As a result, they lose excitement and do not have orgasm. They become increasingly anxious about whether they will achieve orgasm. Anxiety interferes with the sexual response cycle, and orgasm does not occur.
Treatment involves sensate focus. By learning to focus on the sensations that occur, the patient learns not to focus on anxiety or assume the spectator frame of mind.
When the patient reports “no desire” but describes aversion behavior, inhibited desire is typically a conditioned response to the experience of pain during intercourse. Pain—from any cause—during sexual intercourse, can begin a conditioned response that requires recognition, treatment, and, often, counseling to eliminate.
How can the Ob/Gyn help? Therapy model: P LI SS IT
Permission giving. Many sexual problems can be solved by permission-giving. A patient might be bored and wish to try new positions; permission may be all that is required.
LImited information. A patient might have orgasm with masturbation but not penetration. Explaining to the patient that 50% of women do not have orgasm with penetration alone and that it is OK to combine manual stimulation with penetration may be all that is needed.
Specific Suggestions. A patient on decongestants may note decreased lubrication. Use of a lubricant might help. A patient with the “busy mother syndrome” may need specific instruction to make time for a relationship.