Evaluation of Methadone-Induced QTc Prolongation in a Veteran Population
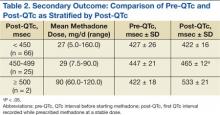
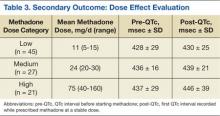
For the primary outcome, the mean pre-QTc and post-QTc were compared. These QTc intervals were further analyzed as secondary outcomes. The mean pre-QTc and post-QTc were compared when stratified by post-QTc of < 450 msec, 450 msec to 499 msec, and ≥ 500 msec. To analyze the dose effect of methadone, the mean pre-QTc and post-QTc were compared when stratified by methadone total daily dose: low (≤ 15 mg/d), medium (16-30 mg/d), and high (> 30 mg/d). Dose ranges were based on typical SAVAHCS prescriptions.
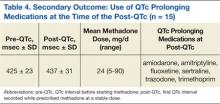
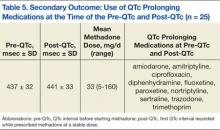
An additional secondary outcome was to determine the effect of the concurrent use of QTc prolonging medications on the QTc interval. The medications the subject was taking at the time of each ECG were reviewed to determine whether any of the medications were listed as Drugs with a risk of Torsades de Pointes or Drugs with a conditional risk of Torsades de Pointes on the CredibleMeds website.22,23 Drugs with a conditional risk of TdP are defined as drugs in which there is evidence that the drug prolongs the QTc interval and has a risk of TdP but only under certain conditions, such as high doses or drug interactions. The mean pre-QTc with and without concurrent use of QTc prolonging medications was compared with the mean post-QTc with QTc prolonging medications in addition to methadone.
Because methadone is extensively metabolized by cytochrome P450 3A4 (CYP3A4), another outcome was to determine the effect of the concurrent use of strong CYP3A4 inhibitors on the QTc interval. The medications the subject was taking at the time of each ECG were reviewed to determine whether any of the medications were listed as strong CYP3A4 inhibitors in The Pharmacist’s Letter/The Prescriber’s Letter.24 The mean pre-QTc with and without the concurrent use of strong CYP3A4 inhibitors was compared with the mean post-QTc with strong CYP3A4 inhibitors in addition to methadone.
Related: Pharmacist-Managed Collaborative Practice for Chronic Stable Angina
The primary and secondary outcomes were compared using a paired t test and descriptive statistics; demographics were analyzed using descriptive statistics. Based on the findings of a previous study, a minimum of 8 patients were needed to meet a power of 0.8 with an alpha 0.05 and a medium effect size when comparing the mean pre-QTc and post-QTc for the primary outcome.25
Results
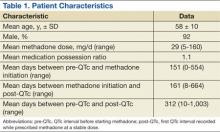
Of 893 EMRs reviewed, 93 met inclusion criteria (Figure 1). The main reason for exclusion was lack of pre-QTc and/or post-QTc (n = 544). The mean age was 58 years (± 10 years), 92% were male, and the mean daily methadone dose at the time of the post-QTc was 29 mg (5 mg-160 mg) (Table 1). Thirty patients were prescribed ≥ 1 QTc prolonging medication at the time of the pre-QTc, 40 patients were prescribed ≥ 1 QTc prolonging medication at the time of the post-QTc, and 0 patients were prescribed a strong CYP3A4 inhibitor at the time of either QTc. There was an average of 151 days (0-554 days) between the pre-QTc and methadone initiation, 161 days (8-664 days) between methadone initiation and the post-QTc, and 312 days (10-1,003 days) between the pre-QTc and post-QTc.
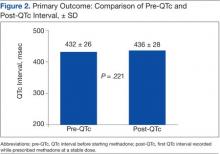
For the primary outcome, there was no significant increase in the QTc interval when comparing the pre-QTc and post-QTc (432 ± 26 msec vs 436 ± 28 msec, P = .221) (Figure 2). When stratified by post QTc, the group of patients with a post-QTc < 450 msec (n = 66) and the group with a post-QTc of ≥ 500 msec (n = 2) had no significant increase in the QTc interval (427 ± 26 msec vs 422 ± 16 msec and 422 ± 18 msec vs 533 ± 21 msec, respectively; P > .05) (Table 2). For the group of patients with a post-QTc of 450 msec to 499 msec (n = 25), methadone significantly prolonged the QTc interval (447 ± 21 msec vs 465 ± 12 msec, P < .001).
When stratified by methadone daily dose of ≤ 15 mg (n = 45), 16 mg to 30 mg (n = 27), and > 30 mg (n = 21), methadone did not significantly prolong the QTc interval in any group (428 ± 29 msec vs 430 ± 25 msec, 436 ± 16 msec vs 439 ± 21 msec, 437 ± 29 msec vs 446 ± 39 msec, respectively; P > .05) (Table 3). For the group of patients using ≥ 1 QTc prolonging medication at the time of the post-QTc and no QTc prolonging medications at the time of the pre-QTc, the addition of methadone did not significantly increase the QTc interval when compared with the pre-QTc (n = 15; 425 ± 23 msec vs 437 ± 31 msec, respectively; P > .05) (Table 4). For the group of patients prescribed ≥ 1 QTc prolonging medication at the pre-QTc and post-QTc, methadone did not significantly prolong the QTc interval (n = 25; 437 ± 32 msec vs 441 ± 33 msec, respectively; P > .05) (Table 5). No subjects were using strong CYP3A4 inhibitors; therefore, the effect of strong CYP3A4 inhibitors could not be assessed.