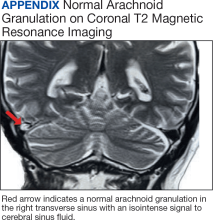
Uncommon Locations for Brain Herniations Into Arachnoid Granulations: 5 Cases and Literature Review
Background: Arachnoid granulations are extensions of the subarachnoid space, an important component of the complex circulation of brain cerebrospinal fluid. While these structures primarily transmit cerebrospinal fluid into the dural venous sinuses, they also may serve as a conduit for brain tissue herniation. Such occurrences have been referred to in the literature as brain herniations into arachnoid granulations (BHAGs), which are considered incidental and asymptomatic but can be associated with nonspecific neurologic symptoms such as headache, tinnitus, vertigo, and seizure. BHAGs can be visualized more readily due to improved cross-sectional magnetic resonance imaging (MRI) with increased spatial and contrast resolution.
Case Presentation: We present 5 cases where brain herniations were detected in patients undergoing MRI for various neurologic symptoms. All patients experienced chronic symptoms, including headaches and seizures. Two cases included BHAG in locations that were associated with the patients’ symptoms.
Conclusions: BHAGs are increasingly recognized due to improved spatial resolution in MRIs. While there is still no definitive evidence that these lesions are responsible for various neurologic symptoms, some of these abnormalities may hold clinical significance such as the visual symptoms seen in 2 of the cases described. BHAG can be associated with gliosis of adjacent brain tissue, which may be a mechanism for symptom development.
CONCLUSIONS
Understanding the clinical impact of brain herniations is important because they are probably more common than previously thought. Improved MRI capabilities suggest that more BHAG will be detected moving forward as radiologists interpret images with higher resolution and thinner slices. Until its significance is fully understood, BHAG will continue to complicate the diagnosis of patients with neurologic complaints whose brain MRIs and EEGs are otherwise unremarkable.
There have been no cases of surgical BHAG intervention and pathology analysis that would help determine their clinical significance. A related entity, temporal lobe encephalocele, has been linked to focal temporal lobe epilepsy, which has demonstrated significant symptom improvement following surgical correction.15 However, encephaloceles have been distinguished from BHAG in part because they do not necessarily herniate through an arachnoid granulation.8 BHAG has only begun to be characterized in detail over the last decade, so more research is needed to understand how it develops and what clinical significance it truly holds.