Bridging the Gap Between Inpatient and Outpatient Care
Background: The Olin E. Teague Veterans’ Center (OETVC) is a teaching hospital with a medical ward consisting of 189 beds, 3 teaching teams with 1 resident and 2 to 3 interns, and 3 nonteaching teams. Due to the complexity of hospitalization, there are concerns that patients may not follow up with primary care or fill their prescribed medication and may have postdischarge questions.
Observations: A program was created at OETVC to bridge the gap between inpatient and outpatient care. Internal medicine residents call all teaching team patients a week following discharge. They discuss medications, changes in symptoms, follow-up plans, and address all questions. The residents also assist with missed orders and make treatment regimen changes if necessary.
Conclusions: This new program has proven to be beneficial. Residents are developing a better understanding of illness scripts and are working on communication skills without time constraints. Patients now have access to a physician following discharge to discuss any concerns with their hospitalization, present condition, and follow-up. Data show a decreased 30-day readmission rate at 6% in the transition of care group compared to 10% in all patients who participated in the program. This program will continue to address barriers to care and adapt to improve the success of care transitions.
Program Description
At the beginning of each week, second- and third-year residents review the list of discharges from the 3 teaching teams. The list is generated by a medical service management analyst. The residents review patient records for inpatient services, laboratory results, medication changes, and proposed follow-up plans designed by the admission team prior to their phone call. The resident is also responsible for reviewing and reconciling discharge instructions and orders. Then, the resident calls the patient and reviews their hospitalization. If a patient does not answer, the resident leaves a voicemail that complies with the Health Insurance Portability and Accountability Act.
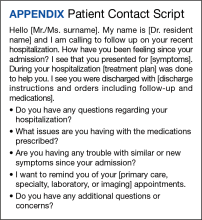
When patients answer the call, the resident follows a script (Appendix). Residents are encouraged to ask patients open-ended questions and address any new needs. They also discuss changes in symptoms, medications, functional status, and remind the patient about follow-up appointments. If imaging or specific orders were missed at discharge, the residents notify the chief resident, lead hospitalist, or deputy associate chief of staff for medical service. If additional laboratory tests need to be ordered, the resident devises a follow-up plan. If needed, specialty referrals can be placed. When residents feel there are multiple items that need to be addressed or if they notice any major concerns, they can recommend the patient present to the emergency department for evaluation. The chief resident, lead hospitalist, and deputy associate chair for medical service are available to assist with discussions about complex medical situations or new concerning symptoms. Residents document their encounters in the Computerized Patient Record System health record and any tests that need follow-up. This differs from the standard of care follow-up programs, which are conducted by primary care medicine nurses and do not fully discuss the hospitalization.
Implementation
This program was implemented as a 1-week elective for interested residents and part of the clinic rotation. The internal medicine medical service analyst pulls all discharges on Friday, which are then provided to the residents. The residents on rotation work through the discharges and find teaching team patients to follow up with and call.
Findings
Implementation of this program has yielded many benefits. The reminder of the importance of a primary care appointment has motivated patients to continue following up on an outpatient basis. Residents were also able to capture lapses in patient understanding. Residents could answer forgotten questions and help patients understand their admission pathology without time pressures. Residents have identified patients with hypoglycemia due to changed insulin regimens, set up specialist follow-up appointments, and provided additional education facilitating adherence. Additionally, several residents have expressed satisfaction with the ability to practice their communication skills. Others appreciated contributing to future patient successes.
While the focus on this article has been to share the program description, we have tabulated preliminary data. In January 2023, there were 239 internal medicine admissions; 158 admissions (66%) were teaching team patients, and 97 patients (61%) were called by a resident and spoken to regarding their care. There were 24 teaching team readmissions within 30 days, and 10 (42%) received a follow-up phone call. Eighty-one admitted patients were treated by nonteaching teams, 10 (12%) of whom were readmissions. Comparing 30-day readmission rates, 10 nonteaching team patients (12%), 10 teaching team patients (6.3%) who talk to a resident in the transition of care program were readmitted, and 24 teaching team patients who did not talk to a resident (10%) were readmitted.