Small Fiber Neuropathy in Veterans With Gulf War Illness
Background: Gulf War veterans deployed to operations Desert Shield and Desert Storm returned with chronic multisystemic symptoms. This Gulf War Illness (GWI) has defied attempts to identify an underlying etiology. Pain and other symptoms attributable to autonomic nervous system (ANS) dysfunction are common, which may suggest a pathophysiologic underpinning.
Methods: A retrospective chart review of clinical data at the New Jersey War Related Illness and Injury Study Center addressed the following questions: (1) how common was biopsy-confirmed SFN in veterans with GWI; (2) do veterans with GWI and SFN report more symptoms attributable to ANS dysfunction as compared to veterans with GWI and no SFN; and (3) can SFN in veterans with GWI and SFN be explained by conditions commonly associated with SFN? Chart review abstracted GWI status, skin biopsy results, and ANS symptom burden. For veterans with GWI and SFN, additional chart abstraction was explored for commonly reported contributing conditions.
Results: From March 1, 2015, to January 31, 2019, 51 Gulf War veterans evaluated at the War Related Illness and Injury Study Center had a skin biopsy. Of these, 42 (83%) were diagnosed with GWI and 24 of 42 (57%) also had SFN. No differences were observed in ANS symptoms when compared with veterans with GWI and no SFN. A potential etiology for SFN was identified in 16 of 24 (67%) veterans with GWI and SFN, increasing to 19 (79%) when hyperlipidemia was included. Our analysis did not identify an explanation in 5 of 24 (21%) veterans with GWI and SFN.
Conclusions: SFN was common in this clinical sample of veterans diagnosed with GWI. A well-established potential etiology was identified in most cases of SFN. About 20% of veterans with GWI in our clinical sample had idiopathic SFN, and it is plausible that deployment-related exposures could have contributed to this condition. Symptoms of ANS are prevalent in GWI, though SFN cannot solely account for this. Our study does not generally support SFN as etiologic for GWI, though this may still be relevant for some. Additional research is required to explore relationships between Gulf War exposures and SFN.
Methods
A retrospective chart review was conducted on veterans evaluated at the WRIISC from March 1, 2015, to January 31, 2019. Inclusion criteria were: deployment to operations Desert Shield and Desert Storm between August 2, 1990, and February 28, 1991, and skin biopsy conducted at the WRIISC. Skin biopsies were obtained at the discretion of an examining clinician based on clinical indications, including neuropathic pain, ANS symptoms, and/or a fibromyalgia/chronic pain–type presentation.
Electronic health record review explicitly abstracted GWI status, results of the skin biopsy, and ANS symptom burden as determined by the Composite Autonomic Symptom Scale 31 (COMPASS 31) completed at the time of the WRIISC evaluation.
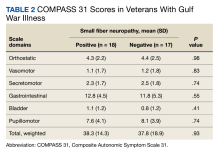
COMPASS 31 assesses symptoms across 6 domains (orthostatic, vasomotor, secretomotor, gastrointestinal, bladder, andpupillomotor). Patients are asked about symptom frequency (rarely to almost always), severity (mild to severe), and improvement (much worse to completely gone). Individual domain scores and a total weighted score (0-100) have demonstrated good validity, reliability, and consistency in SFN.33,34
In veterans with GWI and documented SFN, a health record review was performed to identify potential etiologies for SFN (Appendix).
Statistical Analysis
Microsoft Excel and IBM SPSS 12.0.1 for Windows were used for data collection and statistical analysis. Fisher exact test was used for comparing the prevalence of SFN in veterans with GWI vs without GWI. The independent samples t test was used for comparing COMPASS 31 scores for veterans with GWI by SFN status. α < .05 was used for determining statistical significance. For those GWVs documented with SFN and GWI, potential explanations were documented in total and by condition.
Results
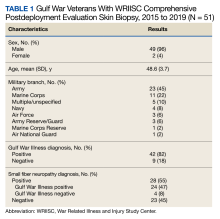
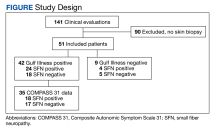
From March 1, 2015, to January 31, 2019, 141 GWVs received a comprehensive in person clinical evaluation at the WRIISC and 51 veterans (36%) received a skin biopsy and were included in this retrospective observational study (Figure). The mean age was 48.6 years, and the majority were male and served in the US Army. Skin biopsies met clinical criteria for GWI for 42 (82%) and 24 of 42 (57%) were determined to have SFN. Four of 9 (44%) veterans without GWI had positive SFN biopsies, though this difference was not statistically significant (Table 1). Veterans with SFN but no GWI were not included in the further analysis.
Thirty-five veterans with GWI—18 with SFN and 17 without SFN—completed the COMPASS 31 (Table 2). COMPASS 31 data were not analyzed for veterans without GWI. Individual domain scores and the difference in COMPASS 31 scores for veterans with GWI and SFN vs GWI and no SFN (38.3 vs 37.8, respectively) were not statistically significant.
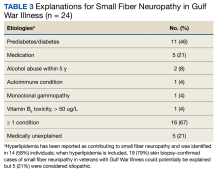
Sixteen of 24 veterans with GWI and SFN (67%) had ≥ 1 conditions that could potentially be responsible for SFN (Table 3), including 11 veterans (46%) with prediabetes/diabetes. Hyperlipidemia is only variably reported as a cause of SFN; when included, 19 of 24 (79%) SFN cases were accounted for. We could not identify a medical explanation for SFN in 5 of 24 veterans (21%) with GWI, which were deemed to be idiopathic.