Moral Injury in Health Care: A Unified Definition and its Relationship to Burnout
Background: Moral injury had been discussed by health care professionals as a cause of occupational distress prior to COVID-19, but the pandemic expanded the appeal and investigation of the term. Moral injury incorporates more than the transdiagnostic symptoms of exhaustion and cynicism and goes beyond operational, demand-resource mismatches of corporatized systems.
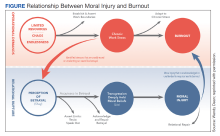
Observations: Moral injury describes the frustration, anger, and helplessness associated with existential threats to a clinician’s professional identity as business interests erode their ability to put patients’ needs ahead of corporate and health system obligations. We propose a framework that combines 2 moral injury definitions. An individual who experiences a betrayal by a legitimate authority has an opportunity to choose their response. Moral injury arises when a superior’s actions or a system’s policies and practices undermine one’s professional obligations to prioritize the patient’s best interest. Perceived as inescapable, the resignation or helplessness of moral injury may present with emotional exhaustion, ineffectiveness, and depersonalization, all hallmarks of burnout. Both moral injury and burnout can mediate and moderate the relationship between triggers for workplace distress and the resulting psychological, existential, and physical harm.
Conclusions: Moral injury is increasingly recognized as a source of distress among health care professionals. It emerges from structural constraints on the ability of health care professionals to deliver optimal care and stand up for patients, their oaths, and their professions. A unified definition of moral injury must be integrated into the framing of clinician distress alongside burnout, recentering health care on ethical decision making rather than profit.
MORAL INJURY AND BURNOUT
In addition to reconciling the definitions of moral injury, the relationship between moral injury and burnout are still being elucidated. We suggest that moral injury and burnout represent independent and potentially interrelated pathways to distress (Figure). Exposure to chronic, inconsonant, and transactional demands, which things like shorter work hours, better self-care, or improved health system operations might mitigate, manifests as burnout. In contrast, moral injury arises when a superior’s actions or a system’s policies and practices—such as justifiable but unnecessary testing, or referral restrictions to prevent revenue leakage—undermine one’s professional obligations to prioritize the patient’s best interest.
If concerns from HCPs about transactional demands are persistently dismissed, such inaction may be perceived as a betrayal, raising the risk of moral injury. Additionally, the resignation or helplessness of moral injury perceived as inescapable may present with emotional exhaustion, ineffectiveness, and depersonalization, all hallmarks of burnout. Both conditions can mediate and moderate the relationship between triggers for workplace distress and resulting psychological, physical, and existential harm.
CONCLUSIONS
Moral injury is increasingly recognized as a source of distress among HCPs, resulting from structural constraints on their ability to deliver optimal care and their own unwillingness to stand up for their patients, their oaths, and their professions.1 Unlike the military, where moral injury is inherent in the contract with society, moral injury in health care (and the relational rupture it connotes) is a signal of systemic dysfunction, fractured trust, and the need for relational repair.
Health care is at a crossroads, experiencing a workforce retention crisis while simultaneously predicting a significant increase in care needs by Baby Boomers over the next 3 decades.
Health care does not have the luxury of experimenting another 30 years with interventions that have limited impact. We must design a new generation of approaches, shaped by lessons learned from the pandemic while acknowledging that prepandemic standards were already failing the workforce. A unified definition of moral injury must be integrated to frame clinician distress alongside burnout, recentering ethical decision making, rather than profit, at the heart of health care. Harmonizing the definitions of moral injury and clarifying the relationship of moral injury with burnout reduces the need for further reinterpretations, allowing for more robust, easily comparable studies focused on identifying risk factors, as well as rapidly implementing effective mitigation strategies.