Nasal Cannula Dislodgement During Sleep in Veterans Receiving Long-term Oxygen Therapy for Hypoxemic Chronic Respiratory Failure
Background: Chronic obstructive pulmonary disease (COPD) is highly prevalent in male veterans. Long-term oxygen therapy (LTOT) can effectively reduce all-cause mortality in these patients, but the effects of nasal cannula dislodgement (NCD) during sleep have not been well studied.
Methods: This study sought to determine whether veterans receiving LTOT for hypoxemic chronic respiratory failure (CRF) due to COPD reported NCD while they slept and, if so, its impact on hospitalizations for COPD exacerbations. Electronic health records were reviewed of veterans with hypoxemic CRF due to COPD who received LTOT and were followed in the pulmonary clinic at the Jesse Brown Veterans Affairs Medical Center between February 1, 2022, and December 31, 2022. Overall hospital cost was calculated for each hospitalized veteran with diagnosed COPD exacerbation. Veterans reported whether they experienced NCD during sleep and, if so, its frequency.
Results
Conclusions
RESULTS
During the study period,
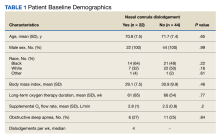
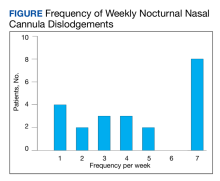
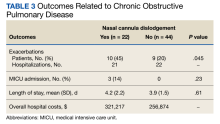
Of the 75 patients, 66 (88%) responded to the telephone survey and 22 patients (33%) reported weekly episodes of NCD while they slept (median, 4 dislodgments per week). (Table 1). Eight patients (36%) reported nightly NCDs (Figure). All 66 respondents were male and 14 of 22 in the NCD group as well as 21 of 44 in the no NCD group were Black veterans. The mean age was similar in both groups: 71 years in the NCD group and 72 years in the no NCD group. There were no statistically significant differences in demographics, including prevalence of obstructive sleep apnea (OSA), supplemental oxygen flow rate, and duration of LTOT, or in pulmonary function test results between patients who did and did not experience NCD while sleeping (Table 2).
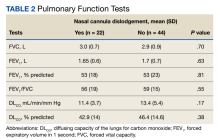
Ten of 22 patients (45%) with NCD and 9 of 44 patients (20%) without NCD were hospitalized at the JBVAMC for ≥ 1 COPD exacerbation in the preceding year that was diagnosed by a physician (P = .045). Three of 22 patients (14%) with NCD and no patients in the no NCD group were admitted to the MICU. No patients required intubation and mechanical ventilation during hospitalization, and no patients died. Overall hospital costs were 25% ($64,342) higher in NCD group compared with the no NCD group and were attributed to the MICU admissions in the NCD group (Table 3). Nine veterans did not respond to repeated telephone calls. One physician-diagnosed COPD exacerbation requiring hospitalization was documented in the nonresponder group; the patient was hospitalized for 2 days. One veteran died before being contacted.