Preparing Veterans Health Administration Psychologists to Meet the Complex Needs of Aging Veterans
Background: There are significant workforce shortages for geriatric mental health care. The imbalance is particularly pronounced in the Veterans Health Administration (VHA) due to the large number of aging veterans receiving care. Workforce-based educational programs are needed to train existing clinicians to meet the mental health needs of aging veterans.
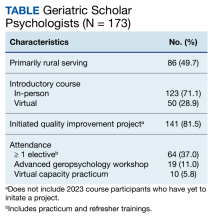
Observations: This article describes an expansion of the Geriatric Scholars Program to train VHA psychologists to care for aging veterans. The multicomponent program includes an introductory course and opportunities to apply geriatric knowledge and skills through quality improvement initiatives. The Geriatric Scholars Program-Psychology Track evolved to incorporate ongoing specialized elective learning opportunities for scholars. A webinar series extends the educational programs to reach the entire VHA workforce.
Conclusions: The Geriatric Scholars Program-Psychology Track represents a longitudinal educational approach to training VHA psychologists in clinical geropsychology. Other community-based organizations can use this model to construct and implement similar programs.
Program description
Introductory Course
Psychologist subject matter experts (SMEs) developed an intensive course in geropsychology in the absence of a similar course in the geriatric medicine board review curriculum. SMEs reviewed the guidelines for practice by professional organizations like the Pikes Peak Geropsychology Competencies,which outline knowledge and skills in various domains.13 SMEs integrated this review with findings from a needs assessment for postlicensed VHA psychology staff in 4 health care systems, drafted a syllabus, and circulated it to geropsychology experts for feedback. The resulting multiday course covered general mental health as well as topics particularly salient for mental health clinicians treating older veterans including suicide prevention and posttraumatic stress disorder (PTSD).14 This Geropsychology Competencies Review Course was piloted in 1 region initially before being offered nationally in 2014.
Quality Improvement
Introductory course attendees also participate in an intensive day-long interactive workshop in quality improvement (QI). After completing these trainings, they apply what they have learned at their home facility by embarking on a QI project related to geriatrics. The QI projects reinforce learning and initiate practice changes not only for attendees but at times the larger health care system. Topics are selected by scholars in response to the needs they observe in their clinics. Recent GSP projects include efforts to increase screenings for depression and anxiety, improve adherence to VHA dementia policy, increase access to virtual care, and increase referrals to programs such as whole health or cognitive behavioral therapy for insomnia, a first-line treatment for insomnia in older adults.17 Another project targeted the improvement of referrals to the Compassionate Contact Corps in an effort to reduce social isolation and loneliness among older veterans.18 Evaluations demonstrate significant improvement in scholars’ confidence in related program development and management from precourse to 3 months postcourse.15
Webinars
The Addressing Geriatric Mental Health webinar series was created to introduce learners to topics that could not be covered in the introductory course. Topics were suggested by the expert reviewers of the curriculum or identified by the scholars themselves (eg, chronic pain, sexuality, or serious mental illness). A secondary function of the webinars was to reach a broader audience. Over time, scholars and webinar attendees requested opportunities to explore topics in greater depth (eg, PTSD later in life). These requests led the webinars to focus on annual themes.
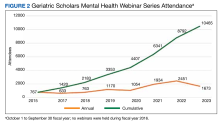
The series is open to all disciplines of geriatric scholars, VHA staff, and non-VHA staff through the Veterans Affairs Talent Management System and the TRAIN Learning Network (train.org). Attendance for the 37 webinars was captured from logins to the virtual learning platform and may underestimate attendance if a group attended on a single screen. Average attendance increased from 157 attendees/webinar in 2015 to 418 attendees/webinar in 2023 (Figure 2). This may have been related to the increase in virtual learning during the COVID-19 pandemic, but represents a 166% increase in audience from the inaugural year of the series.
Advanced Learning Opportunities
To invest in the ongoing growth and development of introductory course graduates, GSP-P developed and offered an advanced workshop in 2019. This multiday workshop focused on further enhancement of geropsychology competencies, with an emphasis on treating older veterans with mental and physical comorbidities. Didactics and experiential learning exercises led by SMEs covered topics such as adjusting to chronic illness, capacity assessment, PTSD, insomnia and sleep changes, chronic pain, and psychological interventions in palliative care and hospice settings. Evaluation findings demonstrated significant improvements from precourse to 6 months postcourse in confidence and knowledge as
To facilitate ongoing and individually tailored learning following the advanced workshop, scholars also developed and executed independent learning plans (ILPs) during a 6-month window with consultation from an experienced geropsychologist. Fifteen of 19 scholars (78.9%) completed ILPs with an average of 3 learning goals listed. After completing the ILPs, scholars endorsed their clinical and/or personal usefulness, citing increased confidence, enhanced skills for use with patients with complex needs, personal fulfillment, and career advancement. Most scholars noted ILPs were feasible and learning resources were accessible. Overall, the evaluation found ILPs to be a valuable way to enhance psychologists’ learning and effectiveness in treating older veterans with complex health needs.20