Implementing a Telehealth Shared Counseling and Decision-Making Visit for Lung Cancer Screening in a Veterans Affairs Medical Center
Background: Veterans suffer substantial morbidity and mortality from lung cancer. Lung cancer screening (LCS) with low-dose computed tomography (LDCT) can reduce mortality. Guidelines recommend counseling and shared decision-making (SDM) to address the benefits and harms of screening and the importance of tobacco cessation before patients undergo screening.
Observations: We implemented a centralized LCS program at the Iowa City Veterans Affairs Medical Center with a nurse program coordinator (NPC)–led telephone visit. Our multidisciplinary team ensured that veterans referred from primary care met eligibility criteria, that LDCT results were correctly coded by radiology, and that pulmonary promptly evaluated abnormal LDCT. The NPC mailed a decision aid to the veteran and scheduled a SDM telephone visit. We surveyed veterans after the visit using validated measures to assess knowledge, decisional conflict, and quality of decision making. We conducted 105 SDM visits, and 91 veterans agreed to LDCT. Overall, 84% of veterans reported no decisional conflict, and 59% reported high-quality decision making. While most veterans correctly answered questions about the harms of radiation, false-positive results, and overdiagnosis, few knew when to stop screening, and most overestimated the benefit of screening and the predictive value of an abnormal scan. Tobacco cessation interventions were offered to 72 currently smoking veterans.
Conclusions: We successfully implemented an LCS program that provides SDM and tobacco cessation support using a centralized telehealth model. While veterans were confident about screening decisions, knowledge testing indicated important deficits, and many did not engage meaningfully in SDM. Clinicians should frame the decision as patient centered at the time of referral, highlight the importance of SDM, and be able to provide adequate decision support.
Evaluating Shared Decision Making
We audio taped and transcribed randomly selected SDM encounters to assess fidelity with the 2016 CMS required discussion elements for counseling about lung cancer, including the benefit of reducing lung cancer mortality; the potential for harms from false alarms, incidental findings, overdiagnosis, and radiation exposure; the need for annual screening; the importance of smoking cessation; and the possibility of undergoing follow-up testing and diagnostic procedures. An investigator coded the transcripts to assess for the presence of each required element and scored the encounter from 0 to 7.
We also surveyed veterans completing SDM, using a convenience sampling strategy to evaluate knowledge, the quality of the SDM process, and decisional conflict. Initially, we sent mailed surveys to subjects to be completed 1 week after the SDM visit. To increase the response rate, we subsequently called patients to complete the surveys by telephone 1 week after the SDM visit.
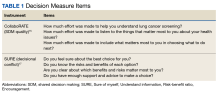
We used the validated LCS-12 knowledge measure to assess awareness of lung cancer risks, screening eligibility, and the benefits and harms of screening.14 We evaluated the quality of the SDM visit by using the 3-item CollaboRATE scale (Table 1).15
The NPC also took field notes during interviews to help identify additional SDM issues. After each call, the NPC noted her impressions of the veteran’s engagement with SDM and understanding of the screening issues.
Clinical Outcomes
We used the screening dashboard and CPRS to track clinical outcomes, including screening uptake, referrals for tobacco cessation, appropriate (screening or diagnostic) follow-up testing, and cancer diagnoses. We used descriptive statistics to characterize demographic data and survey responses.
Initial Findings
We conducted 105 SDM telephone visits from November 2020 through July 2022 (Table 2).
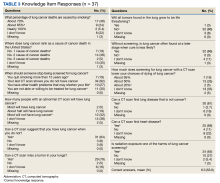
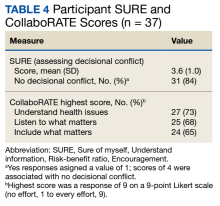
We surveyed 47 of the veterans completing SDM visits (45%) and received 37 completed surveys (79%). All respondents were male, mean age 61.9 years, 89% White, 38% married/partnered, 70% rural, 65% currently smoking, with a mean 44.8 pack-years smoking history. On average, veterans answered 6.3 (53%) of knowledge questions correctly (Table 3).
Only 1 respondent (3%) correctly answered the multiple-choice question about indications for stopping screening. Two (5%) correctly answered the question on the magnitude of benefit, most overestimated or did not know. Similarly, 23 (62%) overestimated or did not know the predictive value of an abnormal scan. About two-thirds of veterans underestimated or did not know the attributable risk of lung cancer from tobacco, and about four-fifths did not know the mortality rank of lung cancer. Among the 37 respondents, 31 (84%) indicated not having any decisional conflict as defined by a score of 4 on the SURE scale.