Pharmacist-Led Antimicrobial Stewardship and Antibiotic Use in Hospitalized Patients With COVID-19
Background: During the COVID-19 pandemic, a significant increase in the use of empiric antibiotic therapy has been observed especially in patients hospitalized with COVID-19. Improving antibiotic prescribing is one of the main goals of the antimicrobial stewardship program (ASP). The ASP pharmacists have a scope of practice that authorizes changes in anti-infective therapy.
Methods: We aimed to describe antibiotic prescribing in patients hospitalized with COVID-19 at Veterans Affairs Southern Nevada Healthcare System with a pharmacist-led ASP and to determine the prevalence of bacterial coinfection in this patient population. We performed a retrospective chart review of patients admitted to the facility from November 1, 2020, to January 31, 2021.
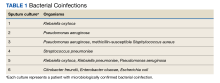
Results: A total of 199 patients were admitted to the hospital for laboratory-confirmed COVID-19 infection during the study period and 61 patients (31%) received ≥ 1 antibiotic on hospital admission and 138 (69%) did not receive antibiotics. Forty-seven patients (77%) had antibiotics discontinued by the ASP team within 72 hours of admission. Of the 199 admitted, 6 (3%) had microbiologically confirmed bacterial coinfection. Pseudomonas aeruginosa was the most common organism (3 sputum cultures) followed by Klebsiella oxytoca (2 sputum cultures). Sixteen patients (8%) developed a nosocomial infection during their hospital stay.
Conclusions: Up to 31% of patients hospitalized for COVID-19 infection received empiric antibiotic treatment for concern of bacterial coinfection. Pharmacist-led ASP led to early discontinuation of antibiotics in many patients. A thorough clinical workup to determine the risk of bacterial coinfection in patients with COVID-19 is important before starting empiric antibiotic therapy. It is essential to continue promoting the ASP during the COVID-19 pandemic to ensure responsible antibiotic use and prevent antimicrobial resistance.
Methods
This retrospective descriptive study included patients who were hospitalized for the treatment of laboratory-confirmed COVID-19 infection. The Theradoc clinical surveillance system was used to retrieve a list of patients who were admitted to VASNHS from November 1, 2020, to January 31, 2021, and tested positive for COVID-19. Patients with incidental positive COVID-19 test results or those who received antibiotics for extrapulmonary indications on hospital admission were excluded.
Each patient chart was reviewed and data, including clinical presentations, procalcitonin (PCT), the requirement of supplemental oxygen, vital signs, imaging findings, antibiotic orders on admission, ASP interventions such as discontinuation or changes to antibiotic therapy during the first 72 hours of hospital admission, clinical outcomes, culture results, and readmission rate, defined as any hospital admission related to COVID-19 or respiratory tract infection within 30 days from the previous discharge, were collected.
The primary objective of the study was to describe antibiotic prescribing in patients hospitalized with COVID-19. The secondary outcomes included the prevalence of bacterial coinfection and nosocomial bacterial infection in patients hospitalized with COVID-19.
Results
A total of 199 patients were admitted to the hospital for laboratory-confirmed COVID-19 infection from November 1, 2020, to January 31, 2021. Sixty-one patients (31%) received at least 1 antibiotic on hospital admission. Among those patients who received empiric antibiotic treatment, 29 patients (48%) met the Systemic Inflammatory Response Syndrome (SIRS) criteria. Fifty-six patients (92%) had ≥ 1 PCT level obtained, and 26 of those (46%) presented with elevated PCT levels (PCT > 0.25). Fifty patients (82%) required oxygen supplement and 49 (80%) presented with remarkable imaging findings. Of 138 patients who did not receive empiric antibiotic therapy within 72 hours of hospital admission, 56 (41%) met the SIRS criteria, 31 (29%) had elevated PCT levels, 100 (72%) required oxygen supplement, and 79 (59%) presented with remarkable imaging findings.
Antibiotic Prescribing
Forty-six of 61 patients (75%) received antibiotic treatment for community-acquired pneumonia (CAP) that included ceftriaxone and azithromycin. Three patients (5%) received ≥ 1 broad-spectrum antibiotic (4th generation cephalosporin [cefepime] or piperacillin-tazobactam), 2 (3%) received vancomycin, and 1 (2%) received a fluoroquinolone (levofloxacin) on admission.
Among 61 patients who received empiric antibiotics, the readmission rate was 6%. The mortality rate was 20%, and the mean (SD) duration of hospital stay was 13.1 (12.5) days.
Six of 199 patients (3%) had microbiologically confirmed bacterial coinfection on hospital admission: 3 were Pseudomonas aeruginosa (P aeruginosa) and 2 were Klebsiella oxytoca (Table 1).