Longitudinal Dynamic in Weight Loss Impacts Clinical Outcomes for Veterans Undergoing Curative Surgery for Colorectal Cancer
Background: Definitions of malnutrition imperfectly reflect nutritional status or predict perioperative consequences. We sought to identify predictive nutritional trends by examining the effect of preoperative weight on postoperative outcomes in patients with colorectal cancer (CRC).
Methods: This retrospective review examined 148 patients with CRC treated with curative-intent surgery at the Veterans Affairs Ann Arbor Healthcare System in Michigan from January 1, 2015 to December 31, 2019. We evaluated weight dynamics of patients, starting 1 year before cancer diagnosis until 1 year after surgery. We evaluated the association of these weight dynamics with surgical outcomes. Primary outcomes observed were hospital readmission and length of stay (LOS), chemotherapy completion, and delayed recovery defined as abnormal clinical developments.
Results: There were 115 patients in the colon cancer (CC) cohort and 33 in the rectal cancer (RC) cohort. Low preoperative albumin (< 3.5 g/dL) was present in 25 patients with CC (22%) and 11 patients with RC (33%). Six-month preoperative weight loss of at least 3% occurred in 32 patients with CC (36%). Delayed recovery was observed in 35 patients with CC (30%) and 21 patients with RC (64%). Nutrition consultation rates for the CC and RC groups were 15% and 36%, respectively, before the operation; 95% and 100%, respectively, for postoperative inpatients; and 12% and 73%, respectively, for postoperative outpatients. Six-month preoperative weight loss of ≥ 3% was significantly associated with delayed recovery (P < .001) and 60-day readmissions (P = .015) but not increased LOS or chemotherapy noncompletion.
Conclusions: A ≥ 3% weight loss 6 months preceding curative surgery for CRC was associated with adverse outcomes. An intensive nutrition prehabilitation program initiated at the time of cancer diagnosis is needed and may reduce associated complications.
Analysis
The data were described using mean (SD) for continuous variables and number and percentages for categorical variables. Where appropriate, Fisher exact test, Pearson χ2 test, Spearman ρ, and Mann-Whitney U test were used for tests of significance. SAS (SAS Institute) was utilized for multivariable analysis. The significance level was P = .05 for all tests.
Results
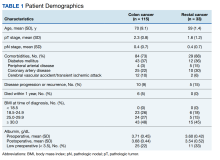
There were 115 patients in the CC cohort and 33 in the RC cohort. The mean (SD) age at diagnosis was 70 (9.1) for CC group and 59 (1.4) for RC group (Table 1).
Weight Trends
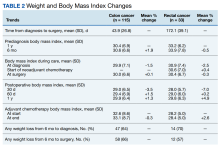
From 1 year to 6 months before diagnosis, 40 of 80 patients lost weight in the CC cohort (mean change, +1.9%) and 6 of 22 patients lost weight in the RC cohort (mean change, + 0.5%). From 6 months before diagnosis to time of diagnosis, 47 of 74 patients lost weight in the CC cohort (mean change, -1.5%) and 14 of 21 patients lost weight in the RC cohort (mean change, -2.5%). From time of diagnosis to time of surgery, 36 of 104 patients with CC and 14 of 32 patients with RC lost weight with a mean weight change of and +0.1% and -0.3%, respectively. In the 6 months before surgery, any amount of weight loss was observed in 58 patients (66%) in the CC group and in 12 patients (57%) in the RC group. In this time frame, in the CC cohort, 32 patients (36%) were observed to have at least 3% weight loss, and 23 (26%) were observed to have at least 5% weight loss (Table 3).
In patients who completed adjuvant chemotherapy in the CC group, mean (SD) BMI at the beginning and end of chemotherapy was 32.6 (8.6) and 33.1 (8.7), respectively, and a -0.3% mean change in weight was observed. In the RC group, mean (SD) BMI was 28.2 (5.0) at the initiation of adjuvant chemotherapy and 28.4 (5.0) at its completion, with a +2.6% mean change in weight.
In the immediate postoperative period, most patients were losing weight in both the CC and RC groups (mean, -3.5% and -7.0% at 1 month postoperative, respectively). At 1-year after surgery, patients had modest mean increases in weight: +1.3% for patients with CC and +4.9% for patients with RC.
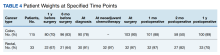
A relatively large proportion of patients had missing data on weights at various data points (Table 4).