High-Grade Staphylococcus lugdunensis Bacteremia in a Patient on Home Hemodialysis
Background: Staphylococcus lugdunensis (S lugdunensis) is a species of coagulase-negative Staphylococcus and a constituent of human skin flora. S lugdunensis has gained notoriety for its virulence, which resembles Staphylococcus aureus (S aureus). S lugdunensis is now recognized as an important nosocomial pathogen and cause of prosthetic device infections, including vascular catheter infections.
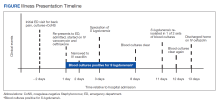
Case Presentation: A 60-year-old man with a history of uncontrolled type 2 diabetes mellitus and end-stage renal disease on home hemodialysis via arteriovenous fistula (AVF) presented to the emergency department for evaluation of subacute progressive low back pain. Initial laboratory tests were notable for elevated inflammatory markers. Magnetic resonance imaging with contrast of the thoracic and lumbar spine revealed abnormal marrow edema in the T11-T12 vertebrae with abnormal fluid signal in the T11-T12 disc space. Cultures grew methicillin-sensitive S lugdunensis. The patient’s antibiotic regimen was narrowed to IV oxacillin. He was transitioned to IV cefazolin dosed 3 times weekly after hemodialysis and an outpatient dialysis center.
Conclusions: Treatment of bacteremia caused by S lugdunensis or S aureus should be managed with prompt initiation of IV antistaphylococcal therapy, a thorough evaluation for the source of bacteremia as well as metastatic complications, and consultation with an infectious disease specialist. This case highlights AVF as a potential source for infection even without localized signs of infection. The buttonhole method of AVF cannulation was thought to be a major contributor to the development and persistence of our patient’s bacteremia. This risk should be discussed with patients using a shared decision-making approach when developing a dialysis treatment plan.
The buttonhole technique is hypothesized to increase infection risk due to the repeated use of the same site for needle entry. Skin flora, including CoNS, may colonize the scab that forms after dialysis access. If proper sterilization techniques are not rigorously followed, the bacteria colonizing the scab and adjacent skin may be introduced into a patient’s bloodstream during needle puncture. Loss of skin integrity due to frequent cannulation of the same site may also contribute to this increased infection risk. It is relevant to recall that our patient received HD 5 times weekly using the buttonhole technique. The use of the buttonhole technique, frequency of his HD sessions, unclear sterilization methods, and immune dysfunction related to his uncontrolled T2DM and renal disease all likely contributed to our patient’s bacteremia.
Using topical mupirocin for prophylaxis at the intended buttonhole puncture site has shown promising results in decreasing rates of S aureus bacteremia.17 It is unclear whether this intervention also would be effective against S lugdunensis. Increasing rates of mupirocin resistance have been reported among S lugdunensis isolates in dialysis settings, but further research in this area is warranted.18
There are no established treatment guidelines for S lugdunensis infections. In vitro studies suggest that S lugdunensis is susceptible to a wide variety of antibiotics. The mecA gene is a major determinant of methicillin resistance that is commonly observed among CoNS but is uncommonly seen with S lugdunensis.5 In a study by Tan and colleagues of 106 S lugdunensis isolates, they found that only 5 (4.7%) were mecA positive.19
Vancomycin is generally reasonable for empiric antibiotic coverage of staphylococci while speciation is pending. However, if S lugdunensis is isolated, its favorable susceptibility pattern typically allows for de-escalation to an antistaphylococcal β-lactam, such as oxacillin or nafcillin. In cases of bloodstream infections caused by methicillin-sensitive S aureus, treatment with a β-lactam has demonstrated superiority over vancomycin due to the lower rates of treatment failure and mortality with β-lactams.20,21 It is unknown whether β-lactams is superior for treating bacteremia with methicillin-sensitive S lugdunensis.
Our patient’s isolate of S lugdunensis was pansensitive to all antibiotics tested, including penicillin. These susceptibility data were used to guide the de-escalation of his empiric vancomycin and ceftriaxone to oxacillin on hospital day 1.