Muscle-Related Adverse Events Associated With PCSK9 Inhibitors in a Veteran Population
Background: Statins and PCSK9 inhibitors (PCSK9i) are used to lower low-density lipoprotein cholesterol and reduce cardiovascular events, yet some patients are unable to tolerate statin therapy due to muscle-related adverse events (AEs). The effect of PCSK9i on muscle-related AEs is not well studied, and available data show inconsistent incidence rates.
Methods: The primary study outcome was to determine the percentage of patients who developed muscle-related PCSK9i AEs. A secondary outcome was to analyze data based on 4 subgroups: tolerated a full PCSK9i dose; tolerated alternative PCSK9i following initial intolerance; required a PCSK9i dose reduction, or discontinued PCSK9i. In addition, the percentage of statin- and/or ezetimibe-intolerant patients in these 4 groups was determined. Another secondary outcome was the management strategies taken for patients who were on a reduced (monthly) dose of PCSK9i who did not reach their low-density lipoprotein cholesterol goal. Statin intolerance was defined as intolerable skeletal muscle AEs on at least 3 different statins. We conducted a single-center, retrospective review of patients prescribed a PCSK9i between December 1, 2017, and September 1, 2021, at a patient aligned care team clinic at the Wilkes-Barre Veterans Affairs Medical Center.
Results: The study included 137 veterans. Twenty-four patients (17.5%) developed a muscle-related AE while on a PCSK9i. In predefined subgroups studied, statin intolerance ranged from 68.1% to 100%, ezetimibe intolerance ranged from 41.6% to 83.3%, and both statin and ezetimibe intolerance ranged from 36.3% to 83.3%.
Conclusions: In this study, muscle-related PCSK9i AEs occurred at a similar incidence rate to that reported in previous clinical trials and exceeded the incidence rate reported in the prescribing information for alirocumab and evolocumab. It also appears that patients who have a prior muscle-related intolerance to a statin and/or ezetimibe have a higher likelihood of developing a muscle-related AE to a PCSK9i.
Results
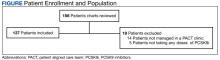
For the study, 156 charts were reviewed and 137 patients were included (Figure).
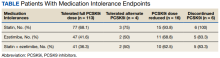
For the secondary results, 4 patients (2.9%) tolerated an alternate PCSK9i (evolocumab 140 mg SQ every 2 weeks) after initial intolerance to PCSK9i, 16 (11.7%) required a dose reduction, and 6 (4.4%) discontinued PCSK9i due to a muscle-related AE.
Statin intolerance was most common in all groups, followed by ezetimibe intolerance, and intolerance to statins + ezetimibe. Of the 113 patients who tolerated a full dose of PCSK9i, 77 (68.1%) had intolerance to statin, 47 (41.6%) to ezetimibe, and 41 (36.3%) to both statins and ezetimibe. Of the 6 patients who discontinued PCSK9i, all had intolerance to statins, 5 (83.3%) to ezetimibe, and 5 (83.3%) to statins and ezetimibe.
For patients who were on a reduced (monthly) dose of a PCSK9i who did not reach their LDL-C goal, we found that 16 patients (11.7%) required a PCSK9i dose reduction following muscle-related AEs. Of the patients who had their dose of PCSK9i reduced to monthly dosing, 5 (31%) met their LDL-C goal. For the 11 patients who did not meet their LDL-C goal, different management strategies were taken. Lifestyle modifications were made in 6 patients (54%), the monthly PCSK9i dose was increased to alirocumab 150 mg SQ monthly in 4 patients (36%), and 1 patient (9.1%) was switched to an alternative PCSK9i. There were no identified muscle-related AEs recorded in patients whose dose was increased to alirocumab 150 mg SQ monthly.
Discussion
This retrospective study found 17.5% of patients experienced muscle-related PCSK9i AEs. These occurred at a higher rate than reported in the prescribing information (< 5%) and were similar to the incidence rates reported in the GAUSS-2, GAUSS-3, and ODYSSEY-ALTERNATIVE clinical trials (12.0%-32.5%), which is what we hypothesized.18,19,22-25 It is important to note that the incidence rates of muscle-related AEs reported in the prescribing information for alirocumab and evolocumab were based on trials that did not include statin- and/or ezetimibe-intolerant patients; whereas many patients in our study and patients in the clinical trials were statin and/or ezetimibe intolerant.