Appropriateness of Pharmacologic Thromboprophylaxis Prescribing Based on Padua Score Among Inpatient Veterans
Background: Hospitalized patients are at increased risk of developing venous thromboembolism (VTE). The Padua Prediction Score (PPS) was developed to help quantify the risk of VTE for hospitalized patients and guide prescribing of pharmacologic thromboprophylaxis. This study aims to assess whether PPS embedded within an admission order set was utilized appropriately to prescribe or withhold pharmacologic thromboprophylaxis.
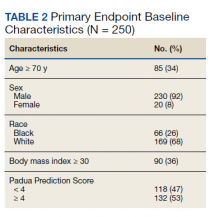
Methods: This single center, retrospective observational cohort study evaluated adult patients aged ≥ 18 years between June 2017 and June 2020. A random sample of 250 patient charts meeting inclusion criteria were reviewed to calculate PPSs, and clinician notes were reviewed for documentation as to whether thromboprophylaxis was given or withheld appropriately based on the PPS. A second cohort of patients admitted within the study period meeting inclusion criteria and readmitted for VTE within 45 days of discharge were evaluated to determine appropriateness of inpatient VTE thromboprophylaxis during index hospitalization based on the PPS.
Results: Of the 250 patients examined, 118 (47.2%) had a PPS < 4 on admission. Of the 118 patients, 58 (49.2%) were inappropriately prescribed pharmacologic thromboprophylaxis administered within 24 hours of admission. The clinical rationale for giving thromboprophylaxis when not indicated was provided for only 2 (3.4%) of the 58 patients. Of the 132 patients with a PPS ≥ 4, 11 (8.3%) had thromboprophylaxis appropriately withheld and for 33 (25.0%) it was inappropriately withheld. A total of 88 (66.7%) patients received thromboprophylaxis as indicated by a PPS ≥ 4.
Conclusions: Despite the inclusion of the PPS calculator in the facility’s admission order set, this study showed pharmacologic thromboprophylaxis was frequently inappropriately given or withheld. This suggests written protocols and order sets may not be solely sufficient to ensure appropriate VTE prophylaxis in actual practice. Incorporation of additional tools, such as dashboards and scorecards, should be explored.
Methods
This was an observational, retrospective cohort study that took place at the US Department of Veterans Affairs (VA) Tennessee Valley Healthcare System (TVHS). TVHS is a multisite health care system with campuses in Nashville and Murfreesboro. Clinical pharmacists employed at the study site and the primary research investigators designed this study and oversaw its execution. The study was reviewed and deemed exempt as a quality improvement study by the TVHS Institutional Review Board.
This study included adult veterans aged ≥ 18 years admitted to a general medicine floor or the medical intensive care unit between June 1, 2017, and June 30, 2020. Patients were excluded if they were on chronic therapeutic anticoagulation prior to their index hospitalization, required therapeutic anticoagulation on admission for index hospitalization (ie, acute coronary syndrome requiring a heparin drip), or were bedded within the surgical intensive care unit. All patients admitted to the TVHS within the prespecified date range were extracted from the electronic health record. A second subset of patients meeting inclusion criteria and readmitted for VTE within 45 days of index hospitalization with International Classification of Diseases, Tenth Revision (ICD-10) descriptions including thrombosis or embolism were extracted for review of a secondary endpoint. Patients with preexisting clots, history of prior DVT or PE, or history of portal vein thrombosis were not reviewed.
The primary endpoint was the percentage of patients for whom pharmacologic thromboprophylaxis was appropriately initiated or withheld based on a PPS calculated upon admission (Table 2). PPS was chosen for review as it is the only RAM currently used at TVHS. Secondary endpoints were the percentage of patients with documented rationale for ordering thromboprophylaxis when not indicated, based on PPS, or withholding despite indication as well as the number of patients readmitted to TVHS for VTE within 45 days of discharge with IMPROVEDD scores ≥ 4 and < 4 (eAppendix available at doi:10.12788/fp.0291). The primary investigators performed a manual health record review of all patients meeting inclusion criteria. Descriptive statistics were used given this was a quality improvement study, therefore, sample size and power calculations were not necessary. Data were stored in Microsoft Excel spreadsheets that were encrypted and password protected. To maintain security of personal health information, all study files were kept on the TVHS internal network, and access was limited to the research investigators.
Results
Two hundred fifty patients meeting inclusion criteria were randomly selected for review for the primary endpoint. Of the patients reviewed for the primary endpoint, 118 had a PPS < 4 and 132 a PPS ≥ 4 (Figure). Pharmacologic thromboprophylaxis was inappropriately given or withheld based on their PPS for 91 (36.4%) patients. This included 58 (49.2%) patients in the low-risk group (PPS < 4) who had thromboprophylaxis inappropriately given and 33 (25.0%) patients in the high-risk group (PPS ≥ 4) who had thromboprophylaxis inappropriately withheld. Of the 58 patients with a PPS < 4 who were given prophylaxis, only 2 (3.4%) patients had documented rationale as to why anticoagulation was administered. Of the 132 patients with a PPS ≥ 4, 44 patients had thromboprophylaxis withheld. Eleven (8.3%) patients had thromboprophylaxis appropriately withheld due to presence or concern for bleeding. Commonly documented rationale for inappropriately withholding thromboprophylaxis when indicated included use of sequential compression devices (40.9%), pancytopenia (18.2%), dual antiplatelet therapy (9.1%), or patient was ambulatory (4.5%).