Virtual Respiratory Urgent Clinics for COVID-19 Symptoms
Background: The COVID-19 pandemic has forced a shift from in-person to virtual care to reduce exposure risks to patients and health care workers. This report aims to describe a large primary care system’s implementation of virtual respiratory urgent care clinics (VRUCs).
Methods: The VA Connecticut Healthcare System (VACHS) delivers care to more than 58,000 veterans in at 8 primary care sites. VRUCs were established as part of the VACHS primary care rapid transition to virtual care model. Retrospective analysis and qualitative chart reviews were performed from February 2020 through May 2020 to describe characteristics of patients who received care through the VRUCs.
Results: VRUCs were used by > 445 patients, 51% received COVID-19 testing, 10% tested positive, 5% were admitted to the hospital, and 18% had ≥ 1 subsequent emergency department visits. Chart documentation rates of discussion of isolation precautions, high occupational risk, and goals of care were 71%, 25%, and 14%, respectively.
Conclusions: Average wait time for health care provider evaluation was 104 minutes, suggesting VRUCs are an expedient means to provide assessment of COVID-19 symptoms. Use of templated notes may ensure routine counseling about isolation, occupation, and goals of care.
Methods
VACHS consists of 8 primary care sites, including a major tertiary care center, a smaller medical center with full ambulatory services, and 6 community-based outpatient clinics with only primary care and mental health. There are 80 individual PCPs delivering care to 58,058 veterans. VRUCs were established during the COVID-19 pandemic to cover patients across the entire health care system, using a rotational schedule of VA PCPs.
COVID-19 Urgent Clinics Program
Within the first few weeks of the pandemic, VACHS primary care established VRUCS to provide expeditious virtual assessment of respiratory or flu-like symptoms. Using the established telehealth system, the intervention aimed to provide emergent screening, testing, and care to those with potential COVID-19 infections. The model also was designed to minimize exposures to the health care workforce and patients.
Retrospective analysis was performed using information obtained from the electronic health record (EHR) database to describe the characteristics of patients who received care through the VRUCs, such as demographics, era of military service, COVID-19 testing rates and results, as well as subsequent emergency department (ED) visits and hospital admissions. A secondary aim included collection of additional qualitative data via a random sample chart review.
Virtual clinics were established January 22, 2020, and data were analyzed over the next 3 months. Data were retrieved and analyzed from the EHR, and codes were used to categorize the VRUCs.
Results
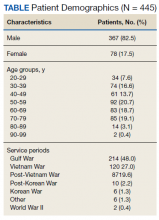
A total of 445 unique patients used these clinics during this period. Unique patients were defined as individual patients (some may have used a clinic more than once but were counted only once). Of this group, 82% were male, and 48% served in the Gulf War era (1990 to present). A total of 51% of patients received a COVID-19 test (clinics began before wide testing availability), and 10% tested positive. Of all patients using the clinics, approximately 5% were admitted to the hospital, and 18% had at least 1 subsequent ED visit (Table).
A secondary aim included review of a random sample of 99 patient charts to gain additional information regarding whether the patient was given appropriate isolation precautions, was in a high-exposure occupation (eg, could expose a large number of people), and whether there was appropriate documentation of goals of care, health care proxy or referral to social work to discuss advance directives. In addition, we calculated the average length of time between patients’ initial contact with the health care system call center and the return call by the PCP (wait time).Of charts reviewed, the majority (71%) had documentation of appropriate isolation precautions. Although 25% of patients had documentation of a high-risk profession with potential to expose many people, more than half of the patients had no documentation of occupation. Most patients (86%) had no updated documentation regarding goals of care, health care proxy, or advance directives in their urgent care VC visit. The average time between the patient initiating contact with the health care system call center and a return call to the patient from a PCP was 104 minutes (excluding calls received after 3:30