Audit and Feedback: A Quality Improvement Study to Improve Antimicrobial Stewardship
Purpose: Many antibiotics prescribed in an outpatient setting may be inappropriate, and by some estimates, half of the antibiotic prescriptions for acute bronchitis may be inappropriate. This quality improvement study aimed to decrease the rate of potentially inappropriate (not guideline concordant) antibiotic prescribing in acute bronchitis.
Methods: This program used an audit and feedback approach. Clinicians received education coupled with audit and feedback, which are components of the Centers of Disease Control and Prevention framework for an effective antimicrobial stewardship program. Antibiotic prescribing rates in patients with acute bronchitis without underlying chronic lung disease or evidence of bacterial infection were compared over two 9-month periods. The baseline period was October 1, 2017 to June 30, 2018 and the posteducation period was October 1, 2018 to June 30, 2019.
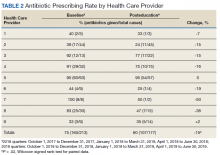
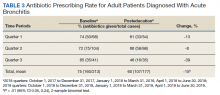
Results: Potentially inappropriate antibiotic prescribing dropped from 75% (160/213) at baseline to 60% (107/177) posteducation (95% CI 0.05, 0.24; P < .01, 2-sample binomial test). Rates were lower for 7 health care providers (HCPs), unchanged for 1 HCP, and slightly increased for 1 HCP between study periods ( P = .02, Wilcoxon signed rank test for paired data).
Conclusions: Study findings show a decline in potentially inappropriate antibiotic prescribing and a resulting improvement in clinic antimicrobial stewardship efforts.
Feedback
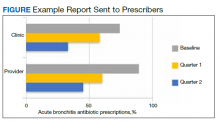
Baseline data were presented to HCPs during the educational session in October 2018. Prospective audits were performed quarterly thereafter (January, April, and July) by the pharmacy resident using the criteria described above. Audit data were compiled into personalized reports and provided to HCPs by the pharmacy resident with written and verbal individual feedback. Written feedback was sent by email to each HCP containing the HCP’s rate, the clinic rate in aggregate, rates from the prior year and quarter(s) for comparison, and clinical pearls from the guidelines (Figure). Verbal feedback included a review of the written feedback and answering any questions concerning the report.
Implementation
Study periods were chosen to coincide with the pharmacy residency training year, which starts in July and ends in June. The start date of October 2018 differed from the start of the residency year (July 2018) owing to delays in obtaining permissions. A&F and analysis of prescribing rates continued through the end of the residency year, for total duration of 9 months (October 1, 2018 to June 30, 2019). For ease of reporting, quarterly reports followed the federal government’s fiscal year (FY) which runs from October 1 of the prior calendar year through September 30 of the year being described. HCPs received 4 feedback reports: baseline (October 1, 2018 - June 30, 2018) in October 2018, quarter 1 (October 1, 2018 - December 31, 2018) in January 2019, quarter 2 (January 1, 2019 - March 31, 2019) in April 2019, and quarter 3 (April 1, 2019 - June 30, 2019) in July 2019.
Statistical Analysis
Prescribing rates were compared between identical 9 -month periods. A 2-sample binomial test for proportions was used to derive an approximate CI of prescribing rates at the patient level. However, to account for clustering of patients within HCP panels and dependence of observations over study periods stemming from examining the same HCPs within each of the periods, the Wilcoxon signed rank test for paired data was used to evaluate prescribing rates at the HCP level. Statistical analysis was performed using R statistical software version 4.0.3. Differences were considered significant at P < .05 set a priori.
This study was approved by the Portland Area Indian Health Service Institutional Review Board (Study ID: 1316730).
Results
All 9 HCPs who see adult patients at the clinic agreed to participate and were all fully present in each study period. Among HCPs, there were 5 physicians and 4 physician assistants or nurse practitioners. There was a total of 213 visits that met study criteria during the baseline period (October 1, 2017 to June 30, 2018) and 177 visits in the posteducation period (October 1, 2018 to June 30, 2019). The total number of acute bronchitis encounters varied by HCP (Ranges, 5-63 [baseline] and 2-57 [posteducation]); however, the relative number of encounters each HCP contributed was similar in each study period (Table 2). The pharmacy resident spent about 2 hours each quarter to generate 9 feedback reports, 1 for each HCP.
Antibiotic Prescribing
Antibiotic prescribing rates decreased from 75% at baseline to 60% at posteducation month 9 (absolute difference, -15% [95% CI, 5 - 24%]; P ≤ .01) (Table 3). The clinic rate was lower for each quarter in FY 2019 (posteducation) compared with the same quarter of FY 2018 (baseline), with the lowest rate observed in the final quarter of the study. Comparing pre- and post- A&F, the rates for HCPs prescribing antibiotics were lower for 7 HCPs, unchanged for 1 HCP, and slightly increased for 1 HCP(P = .02).