Management of Do Not Resuscitate Orders Before Invasive Procedures
Background: In 2017, the US Department of Veterans Affairs (VA) implemented the Life-Sustaining Treatment Decisions Initiative (LSTDI), which created a portable and durable code status for use across its health care system. Patients who now have a durable do not resuscitate (DNR) status may undergo invasive procedures. Few studies have examined whether proceduralists discuss DNR status and document changes before procedures.
Objective: To assess baseline percentage of suspension of DNR before nonsurgical invasive procedures and determine whether an academic detailing intervention consisting of training proceduralists in the use of a template that allows rapid suspension of DNR status increases percentage of DNR acknowledgments.
Methods: Single-center, quasi-experimental pre- and postassessments were done in high-volume, procedural areas, including gastroenterology, cardiology, and interventional radiology, in a VA medical center. The primary outcome was the proceduralists’ documentation of DNR status acknowledgment before a nonsurgical invasive procedure at baseline and after the intervention. Logistic regression was used to compare percentage of DNR acknowledgment with time (before, after) and procedural area and assessing their interaction in the model.
Results: The interaction between department and time revealed wide variation in documentation of DNR acknowledgment. Examining the model predicted percentages from the interaction, preintervention percentages for gastroenterology, cardiology and interventional radiology were 46%, 75.6%, and 7.5%, respectively, and postintervention model predicted percentages were 53.5%, 91.7%, and 26.3%, respectively. Only the before vs after contrast for interventional radiology was significantly different. When all procedural areas were combined, the percentage of DNR acknowledgment significantly improved from 38.6% to 61.1% ( P = .01).
Conclusions: Before nonsurgical invasive procedures, the percentage of DNR acknowledgment was low but after, the intervention significantly improved. Further research is needed to assess its impact on patient-centered outcomes.
The intervention was composed of 2 elements: (1) an addendum to the LST note, which temporarily suspended resuscitation orders (Figure). We developed the addendum based on templates and orders in use before LSTDI implementation. Physicians from the procedural areas reviewed the addendum and provided feedback and the facility chief-of-staff provided approval. Part 2 was an educational presentation to proceduralists in each procedural area. The presentation included a brief introduction to the LSTDI, where to find a life-sustaining treatment note, code status, the importance of addressing code status, and a description of the addendum. The proceduralists were advised to use the addendum only after discussion with the patient and obtaining verbal consent for DNR suspension. If the patient elected to remain DNR, proceduralists were encouraged to document the conversation acknowledging the DNR.
Outcomes
The primary outcome of the study was proceduralist acknowledgment of DNR status before nonsurgical invasive procedures. DNR status was considered acknowledged if the proceduralist provided any type of documentation.
Statistical Analysis
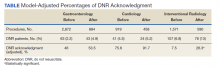
Model predicted percentages of DNR acknowledgment are reported from a logistic regression model with both procedural area, time (before vs after) and the interaction between these 2 variables in the model. The simple main effects comparing before vs after within the procedural area based on post hoc contrasts of the interaction term also are shown.
Results
During the first 6 months following LSTDI implementation (the preintervention phase), 5,362 invasive procedures were performed in gastroenterology, interventional radiology, and cardiology. A total of 211 procedures were performed on patients who had a prior LST note indicating DNR. Of those, 68 (32.2%) had documentation acknowledging their DNR status. The educational presentation was given to each of the 3 departments with about 75% faculty attendance in each department. After the intervention, 1,932 invasive procedures were performed, identifying 143 LST notes with a DNR status. Sixty-five (45.5%) had documentation of a discussion regarding their DNR status.
The interaction between procedural areas and time (before, after) was examined. Of the 3 procedural areas, only interventional radiology had significant differences before vs after, 7.5% vs 26.3%, respectively (P = .01). Model-adjusted percentages before vs after for cardiology were 75.6% vs 91.7% (P = .12) and for gastroenterology were 46% vs 53.5% (P = .40) (Table). When all 3 procedural areas were combined, there was a significant improvement in the overall percentage of DNR acknowledgment postintervention from 38.6% to 61.1.% (P = .01).
Discussion
With the LSTDI, DNR orders remain in place and are valid in the inpatient and outpatient setting until reversed by the patient. This creates new challenges for proceduralists. Before our intervention, only about one-third of proceduralists’ recognized DNR status before procedures. This low rate of preprocedural DNR acknowledgments is not unique to the VA. A pilot study assessing rate of documentation of code status discussions in patients undergoing venting gastrostomy tube for malignant bowel obstruction showed documentation in only 22% of cases before the procedure.10 Another simulation-based study of anesthesiologist showed only 57% of subjects addressed resuscitation before starting the procedure.11
Despite the low initial rates of DNR acknowledgment, our intervention successfully improved these rates, although with variation between procedural areas. Prior studies looking at improving adherence to guidelines have shown the benefit of physician education.12,13 Improving code status acknowledgment before an invasive procedure not only involves increasing awareness of a preexisting code status, but also developing a system to incorporate the documentation process efficiently into the procedural workflow and ensuring that providers are aware of the appropriate process. Although the largest improvement was in interventional radiology, many patients postintervention still did not have their DNR orders acknowledged. Confusion is created when the patient is cared for by a different HCP or when the resuscitation team is called during a cardiac arrest. Cardiopulmonary resuscitation may be started or withheld incorrectly if the patient’s most recent wishes for resuscitation are unclear.14