Examining the Interfacility Variation of Social Determinants of Health in the Veterans Health Administration
Introduction: Recently, numerous studies have linked social determinants of health (SDoH) with clinical outcomes. While this association is well known, the interfacility variability of these risk favors within the Veterans Health Administration (VHA) is not known. Such information could be useful to the VHA for resource and funding allocation. The aim of this study is to explore the interfacility variability of 5 SDoH within the VHA.
Methods: In a cohort of patients (aged ≥ 65 years) hospitalized at VHA acute care facilities with either acute myocardial infarction (AMI), heart failure (HF), or pneumonia in 2012, we assessed (1) the proportion of patients with any of the following five documented SDoH: lives alone, marginal housing, alcohol use disorder, substance use disorder, and use of substance use services, using administrative diagnosis codes and clinic stop codes; and (2) the documented facility-level variability of these SDoH. To examine whether variability was due to regional coding differences, we assessed the variation of living alone using a validated natural language processing (NLP) algorithm.
Results: The proportion of veterans admitted for AMI, HF, and pneumonia with SDoH was low. Across all 3 conditions, lives alone was the most common SDoH (2.2% [interquartile range (IQR), 0.7-4.7]), followed by substance use disorder (1.3% [IQR, 0.5-2.1]), and use of substance use services (1.2% [IQR, 0.6-1.8]). Using NLP, the proportion of hospitalized veterans with lives alone was higher for HF (14.4% vs 2.0%, P < .01), pneumonia (11% vs 1.9%, P < .01), and AMI (10.2% vs 1.4%, P < .01) compared with International Classification of Diseases, Ninth Edition codes. Interfacility variability was noted with both administrative and NLP extraction methods.
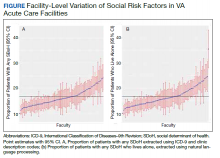
Conclusions: The presence of SDoH in administrative data among patients hospitalized for common medical issues is low and variable across VHA facilities. Significant facility-level variation of 5 SDoH was present regardless of extraction method.
Results
In total, 21,991 patients with either HF (9,853), pneumonia (9,362), or AMI (2,776) were identified across 91 VHA facilities. The majority were male (98%) and had a median (SD) age of 77.0 (9.0) years. The median facility-level proportion of veterans who had any of the SDoH risk factors extracted through administrative codes was low across all conditions, ranging from 0.5 to 2.2%. The most prevalent factors among patients admitted for HF, AMI, and pneumonia were lives alone (2.0% [Interquartile range (IQR), 1.0-5.2], 1.4% [IQR, 0-3.4], and 1.9% [IQR, 0.7-5.4]), substance use disorder (1.2% [IQR, 0-2.2], 1.6% [IQR: 0-3.0], and 1.3% [IQR, 0-2.2] and use of substance use services (0.9% [IQR, 0-1.6%], 1.0% [IQR, 0-1.7%], and 1.6% [IQR, 0-2.2%], respectively [Table]).
When utilizing the NLP algorithm, the documented prevalence of lives alone in the free text of the medical record was higher than administrative coding across all conditions (12.3% vs. 2.2%; P < .01). Among each of the 3 assessed conditions, HF (14.4% vs 2.0%, P < .01) had higher levels of lives alone compared with pneumonia (11% vs 1.9%, P < .01), and AMI (10.2% vs 1.4%, P < .01) when using the NLP algorithm. When we examined the documented facility-level variation in the proportion of individuals with any of the 5 SDoH administrative codes or NLP, we found large variability across all facilities—regardless of extraction method (Figure).
Discussion
While SDoH are known to impact health outcomes, the presence of these risk factors in administrative data among individuals hospitalized for common medical issues is low and variable across VHA facilities. Understanding the documented, facility-level variability of these measures may assist the VHA in determining how it invests time and resources—as different facilities may disproportionately serve a higher number of vulnerable individuals. Beyond the VHA, these findings have generalizable lessons for the US health care system, which has come to recognize how these risk factors impact patients’ health.10
Although the proportion of individuals with any of the assessed SDoH identified by administrative data was low, our findings are in line with recent studies that showed other risk factors such as social isolation (0.65%), housing issues (0.19%), and financial strain (0.07%) had similarly low prevalence.8,11 Although the exact prevalence of such factors remains unclear, these findings highlight that SDoH do not appear to be well documented in administrative data. Low coding rates are likely due to the fact that SDoH administrative codes are not tied to financial reimbursement—thus not incentivizing their use by clinicians or hospital systems.
In 2014, an Institute of Medicine report suggested that collection of SDoH in electronic health data as a means to better empower clinicians and health care systems to address social disparities and further support research in SDoH.12 Since then, data collection using SDoH screening tools has become more common across settings, but is not consistently translated to standardized data due to lack of industry consensus and technical barriers.13 To improve this process, the Centers for Medicare and Medicaid Services created “z-codes” for the ICD-10 classification system—a subset of codes that are meant to better capture patients’ underlying social risk.14 It remains to be seen if such administrative codes have improved the documentation of SDoH.
As health care systems have grown to understand the impact of SDoH on health outcomes,other means of collecting these data have evolved.1,10 For example, NLP-based extraction methods and electronic screening tools have been proposed and utilized as alternative for obtaining this information. Our findings suggest that some of these measures (eg, lives alone) often may be documented as part of routine care in the electronic health record, thus highlighting NLP as a tool to obtain such data. However, other studies using NLP technology to extract SDoH have shown this technology is often complicated by quality issues (ie, missing data), complex methods, and poor integration with current information technology infrastructures—thus limiting its use in health care delivery.15-18
While variance among SDoH across a national health care system is natural, it remains an important systems-level characteristic that health care leaders and policymakers should appreciate. As health care systems disperse financial resources and initiate quality improvement initiatives to address SDoH, knowing that not all facilities are equally affected by SDoH should impact allocation of such resources and energies. Although previous work has highlighted regional and neighborhood levels of variation within the VHA and other health care systems, to our knowledge, this is the first study to examine variability at the facility-level within the VHA.2,4,13,19