Ten-Year Outcomes of a Systems-Based Approach to Longitudinal Amputation Care in the US Department of Veteran Affairs
Background: The goal of the US Department of Veterans Affairs (VA) Amputation System of Care (ASoC) is to enhance the quality and consistency of amputation rehabilitation care for veterans with limb loss.
Objective: The ASoC provides specialized expertise in amputation rehabilitation incorporating the latest practices in medical management, rehabilitation, and artificial limbs in order to minimize disability and to enable the highest level of social, vocational, and recreational success for veterans with amputation.
Discussion: The ASoC serves veterans with limb amputation from any etiology. Between 2009 and 2019, the VA experienced a 34% increase in the number of veterans with amputation who received care. During the same 10-year period, the percentage of veterans with major limb amputation seen in an outpatient amputation specialty clinic each year increased from 4.8 to 26%. This article highlights how the mission of the ASoC has been accomplished over the past decade through prioritization and implementation of key strategic initiatives in learning organization creation, trust in VA care, modernization, and development of a high-performance network with enhanced access and customer service.
Conclusions: This synopsis of the VA amputation care program serves as a model of amputation care that can be utilized outside the federal sector and has the potential to serve as a systems-based example for providing longitudinal care to other populations within the VA.
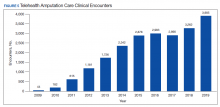
Another unique example is the use of virtual care to see veterans when they are being provided services by a community prosthetist. This service improves the timeliness of care and reduces the travel burden for the veteran. Between 2009 and 2019, total virtual care encounters to provide amputation-related services grew from 44 encounters to 3,905 encounters (Figure 5). In 2019, 13.8% of veterans seen in a VA outpatient amputation specialty clinic had at least 1 virtual encounter in the same year.6
In addition to the expansion of virtual care and building capacity through increasing the number of amputation specialty clinics and providers, the ASoC has used a host of other strategies to improve care access. The development of provider expertise in amputation care has been achieved through the methods of extensive provider training. Implementation of Patient Self-Referral Direct Scheduling allows veterans to access the outpatient amputation specialty clinic without a referral and without having to be seen by their primary care provider. This initiative provides easier and more timely access to amputation specialty services while reducing burden on primary care services. The amputation outpatient specialty clinic was one of a few specialty programs to be an early adopter of national online scheduling. The implementation of this service is still ongoing, but this program gives veterans greater control over scheduling, canceling, and rescheduling appointments.
Conclusions
During the 10 years following its implementation, the VA ASoC has successfully enhanced the quality and consistency of care and rehabilitation services provided to veterans with limb loss through the provision of highly specialized services in the areas of medical care, rehabilitation services, and prosthetic technology. This mission has been accomplished through prioritization and implementation of key strategic initiatives in learning organization creation, trust in VA care, development of a modern, high-performance network, and customer service. Collaborative partnerships both internally within the VA and externally with key stakeholders has facilitated this development, and these will need to be enhanced for future success. Evolving trends in amputation surgery, limb transplantation, artificial limb control and suspension strategies as well as advances in assistive technology also will need to be integrated into best practices and program development.