You Need a Plan: A Stepwise Protocol for Operating Room Preparedness During an Infectious Pandemic
Background: The worldwide spread of SARS-CoV-2, the coronavirus that causes the syndrome designated COVID-19, presents a challenge for emergency operative management. The transmission and virulence of this new pathogen has raised concern for how best to protect operating room staff while effectively providing care to the infected patient requiring urgent or emergent surgery.
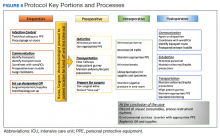
Observations: Establishment of a clear protocol that adheres to rigorous infection control measures while providing a safe system for interfacility transport and operative care is vital to a successful surgical pandemic response. While emergency protocols must be rapidly developed, they should be collaboratively improved and incorporate new knowledge as and when it becomes available. These measures combined with practice drills to keep operating room personnel ready and able should help construct processes that are useful, easy to follow, and tailored to the unique local environment of each health care setting.
Conclusions: After the initial apprehensions and struggles during our confrontation with the COVID-19 crisis, it is our hope that the experience we share will be helpful to surgical staff at other institutions grappling with the challenges of operative care in the pandemic environment. While this protocol focuses on the current COVID-19 pandemic, these recommendations serve as a template for surgical preparedness that can be readily adapted to infectious disease crisis that unfortunately might emerge in the future.
Our experience also highlighted the importance of treating a new protocol as an evolving document, which can be modified and improved through the conduct of training and simulation exercises with providers across disciplines (Figure 6). In gathering nurses, anesthesia staff, and surgeons to perform drills and simulate their roles in an imaginary scenario, we gained new insights, and made corrections and additions that ultimately generated the presently described process. Modifications to any protocol may be necessary depending on the unique circumstances of individual health care systems and hospitals, the characteristics of the patient population they cater to, and the resources and expertise they have available. As the pandemic continues, we are bound to learn more about the epidemiology and modes of transmission of SARS-CoV-2, which may demand further changes to our practice. It is crucial to remember that while emergency policies must be rapidly developed, they should be collaboratively improved and incorporate new knowledge when it becomes available. This is essential to ensure the ultimate protocol is useful, up-to-date, easy to follow and tailored to the unique local environment of each health care setting.
After the initial apprehensions and struggles that attended our confrontation with the crisis, it is our hope that the experience we share will be helpful to surgical staff at other institutions grappling with the challenges of operative care in the pandemic environment. While this protocol focuses on the current COVID-19 pandemic, these recommendations serve as a template for surgical preparedness that can be readily adapted to the next infectious disease crisis that will inevitably emerge.