Initiative to Minimize Pharmaceutical Risk in Older Veterans (IMPROVE) Polypharmacy Clinic
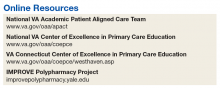
This article is part of a series that illustrates strategies intended to redesign primary care education at the Veterans Health Administration (VHA), using interprofessional workplace learning. All have been implemented in the VA Centers of Excellence in Primary Care Education (CoEPCE). These models embody visionary transformation of clinical and educational environments that have potential for replication and dissemination throughout VA and other primary care clinical educational environments. For an introduction to the series see Klink K. Transforming primary care clinical learning environments to optimize education, outcomes, and satisfaction. Fed Pract. 2018;35(9):8-10.
Planning and Implementation
IMPROVE has its origins in a scholarly project developed by a West Haven CoE physician resident trainee. Development of the IMPROVE program involved VA health psychology, internal medicine faculty, geriatric medicine faculty, NP faculty, and geriatric pharmacy residents and faculty. Planning started in 2013 with a series of pilot clinics and became an official project of the West Haven CoE in September 2014. The intervention required no change in West Haven VAMC policy. However, the initiative required buy-in from West Haven CoE leadership and the director of the West Haven primary care clinic.
Curriculum
IMPROVE is an educational, workplace learning, and clinical activity that combines a 1-hour trainee teaching session, a 45-minute group visit, and a 60-minute individual clinic visit to address the complex problem of polypharmacy. It emphasizes the sharing of trainee and faculty backgrounds by serving as a venue for interprofessional trainees and providers to discuss pharmacologic and nonpharmacologic treatment in the elderly and brainstorm strategies to optimize treatment regimens, minimize risk, and execute medication plans with patients.
All CoEPCE trainees in West Haven are required to participate in IMPROVE and on average, each trainee presents and sees one of their patients at least 3 times per year in the program. Up to 5 trainees participate in each IMPROVE session. Trainees are responsible for reviewing their panels to identify patients who might benefit from participation, followed by inviting the patient to participate. Patients are instructed to bring their pill bottles to the visit. To prepare for the polypharmacy clinic, the trainees, the geriatrician, and the geriatric pharmacist perform an extensive medication chart review, using the medication review worksheet developed by West Haven VAMC providers.4 They also work with a protocol for medication discontinuation, which was compiled by West Haven VAMC clinicians. The teams use a variety of tools that guide appropriate prescribing in older adult populations.5,6 During a preclinic conference, trainees present their patients to the interprofessional team for discussion and participate in a short discussion led by a pharmacist, geriatrician, or health psychologist on a topic related to prescribing safety in older adults or nonpharmacologic treatments.
IMPROVE emphasizes a patient-centered approach to develop, execute, and monitor medication plans. Patients and their family members are invited by their trainee clinician to participate in a group visit. Typically, trainees invite patients aged ≥ 65 years who have ≥ 10 medications and are considered appropriate for a group visit.
The group visit process is based on health psychology strategies, which often incorporate group-based engagement with patients. The health psychologist can give advice to facilitate the visit and optimize participant involvement. There is a discussion facilitator guide that lists the education points to be covered by a designated trainee facilitator and sample questions to guide the discussion.7 A health psychology resident and other rotating trainees cofacilitate the group visit with a goal to reach out to each group member, including family members, and have them discuss perceptions and share concerns and treatment goals. There is shared responsibility among the trainees to address the educational material as well as involve their respective patients during the sessions.
Immediately following the group visit, trainees conduct a 1-hour clinic session that includes medication reconciliation, a review of an IMPROVE questionnaire, orthostatic vital signs, and the St. Louis University Mental Status (SLUMS) exam to assess changes in cognition.7,8 Discussion involved the patient’s medication list as well as possible changes that could be made to the list. Using shared decision-making techniques, this conversation considers the patients’ treatment goals, feelings about the medications, which medications they would like to stop, and AEs they may be experiencing. After the individual visit is completed, the trainee participates in a 10-minute interprofessional precepting session, which may include a geriatrician, a pharmacist, and a health psychologist. In the session they may discuss adjustments to medications and a safe follow-up plan, including appropriate referrals. Trainees discuss the plan with the patient and send a letter describing the plan shortly after the visit.
IMPROVE combines didactic teaching with experiential education. It embodies the 4 core domains that shape the CoEPCE curriculum. First, trainees learn interprofessional collaboration concepts, including highlighting the roles of each profession and working with an interprofessional team to solve problems. Second, CoEPCE trainees learn performance improvement under the supervision of faculty. Third, IMPROVE allows trainees to develop sustained relationships with other team members while improving the quality of the clinic experience as well as with patients through increased continuity of care. Trainees see patients on their panel and are responsible for outreach before and after the visit. Finally, with a focus on personalized patient goals, trainees have the opportunity to further develop skills in shared decision making (SDM).
Related: Reducing Benzodiazepine Prescribing in Older Veterans: A Direct-to-Consumer Educational Brochure
The IMPROVE model continues to evolve. The original curriculum involved an hour-long preclinic preparation session before the group visit in which trainees and faculty discussed the medication review for each patient scheduled that day. This preparation session was later shortened to 40 minutes, and a 20-minute didactic component was added to create the current preclinic session. The didactic component focused on a specific topic in appropriate prescribing for older patients. For example, one didactic lesson is on a particular class of medications, its common AEs, and practical prescribing and “deprescribing” strategies for that class. Initially, the oldest patients or patients who could be grouped thematically, such as those taking both narcotics and benzodiazepines, were invited to participate, but that limited the number of appropriate patients within the CoEPCE. Currently, trainees identify patients from their panels who might benefit, based on age, number of medications, or potential medication-related concerns, such as falls, cognitive impairment, or other concerns for adverse drug effects. These trainees have the unique opportunity to apply learned strategies to their patients to continue to optimize the medication regimen even after the IMPROVE visit. Another significant change was the inclusion of veterans who are comanaged with PCPs outside the VA, because we found that patients with multiple providers could benefit from improved coordination of care.