Reducing the Expenditures and Workload Associated With VA Partial-Fill Prescription Processing
The following equation was used to calculate total partial-fill expenditures for any specified time frame:
Total partial-fill expenditure = total raw drug cost + (material cost × number of partial fills)
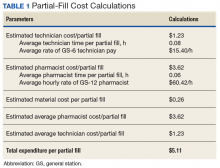
In addition, the average personnel cost per partial-fill prescription was determined. Average workload expenditure per partial fill was calculated by filling a subset of 10 test prescriptions and multiplying the average time spent by an average of the general station (GS) rate for pharmacists and technicians. The average hourly rate of a GS-12 pharmacist was calculated based on an average of the 10 available pay grades within the GS-12 ranking. The average hourly rate of a GS-6 pharmacy technician was calculated based on an average of the 10 available pay grades within the GS-6 ranking.3 The average workload expenditures were calculated using the following equations:
Average pharmacist workload expenditure per partial fill = time (in hours) × average hourly rate.
Average technician workload expenditure per partial fill = time (in hours) × average hourly rate.
Partial-Fill Guidance
Updated partial-fill guidance was drafted designating acceptable prescriptions to be limited to those responsible for preventing hospitalization and treatment of acute illness. This guidance provided generalized examples of medication classes that could be acceptable for partial filling, though it was not intended to be an all-inclusive list. The guidance also noted examples of classes or groups that should not be partial filled for nonemergent reasons (vitamins, nonprescription items, antilipemics), as well as controlled substances. The refill-process education was reiterated throughout the entirety of the guidance. Specifically, if a pharmacy staff member was to perform a partial fill, a review explaining the appropriate refill process to the veteran also must be provided. If the medication was determined to be of emergent need and not yet transmitted for filling via the CMOP, the directive recommended to fill the entire quantity locally as a onetime fill.
If a onetime on-site fill was determined infeasible, partial-fill quantities were recommended to be limited to only a 7-day supply, and the full quantity filled through the CMOP. Anticipated mail wait time for CMOP prescription delivery was estimated to be less than 7 days based on experience, local pending queues, and guidance from the regional CMOP; however, time could vary among VA and CMOP facilities. Original prescriptions were to be filled for the entire quantity for the first fill at the on-site pharmacy if requested by the veteran. If the pharmacy had an insufficient quantity for an entire initial supply, it could then be partial filled for a 7-day supply and then filled through the CMOP.
The final portion of the partial-fill guidance pertained to the use of partial-fill justification codes. Prior to the execution of the partial-fill guidance, free text was entered into the comments field when processing a partial-fill prescription, as the prescription-processing system used requires a comment to proceed with the partial fill. The use of these codes served to streamline data collection in the postintervention phase and helped identify areas for further education following the close of this project.
Education
Education to the pharmacy staff was disseminated by various modalities, including in-person sessions and written and electronic correspondences. This written guidance was distributed to pharmacy staff by e-mail, the pharmacy newsletter (Rx-tra), signage posted throughout the outpatient pharmacies, and on the facility’s pharmacy Microsoft SharePoint (Redmond, WA) site. In-services provided during pharmacy staff meetings detailed information on the updated partial-fill guidance. A FVAMC Talent Management System (TMS) training module was developed and assigned to all pharmacy service staff to reiterate key points regarding this QI initiative (eAppendix).
Nonpharmacy staff were educated through staff and in-service meetings and e-mail correspondences. These in-services emphasized how nurses, medical support assistants, and health care providers (HCPs) could assist veterans by knowing the correct refill process, ensuring sufficient refills remained until the next appointment, and providing continual refill-process education.
Following implementation, all veterans receiving prescriptions through the on-site pharmacies in the FVAMC were provided a copy of the refill-process handout with each trip to the pharmacy. Nonpharmacy staff and HCPs also were provided this handout to distribute to patients. The intent of this handout was to clearly detail the various ways in which refills could be ordered and the time frame in which they should be ordered. The pharmacy became involved in new patient orientation classes for all veterans new to FVAMC. Digital signage and messaging was created and circulated throughout several of the FVAMC facilities.
Results
The results of calculations for material cost, personnel time spent, hourly employee rates, and average workload expenditure per partial fill are summarized in Table 1.
Following the implementation of partial-fill and refill-process education, there was a 54.3% decrease in the total number of partial fills from 5,596 in the 90 days prior to implementation, to 2,555 partials completed over the 90 days postimplementation. Regarding the primary objective, total partial-fill expenditures decreased from $52,015.44 to $44,063.01 (-15.3%). When dissecting the individual components of partial-fill expenditures, material expenditures decreased from $1,454.96 to $664.28 (-54.3%), and raw drug cost expenditures decreased from $50,596.48 to $43,398.73 (-14.3%). Workload expenditures also decreased from $27,140.60 to $12,391.75 (-54.3%).