Outcomes Associated With a Multidisciplinary Pain Oversight Committee to Facilitate Appropriate Management of Chronic Opioid Therapy
Results
Interventions spanned 19 months, with an average of 1 intervention per month. The highest number of POC interventions in a single month was observed in October 2014, with 3 individual interventions from 3 separate categories.
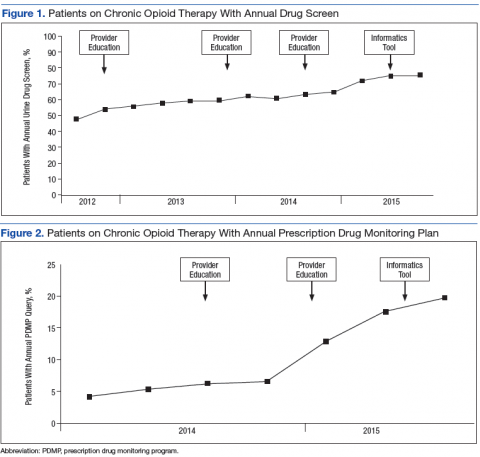
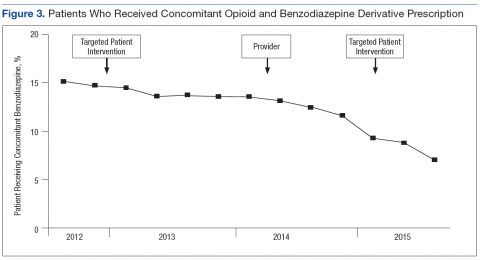
Impact of POC Interventions on COT Monitoring
During the study period, patients meeting COT criteria who received an annual UDS increased from 47.8% to 75.5%, a 56.7% increase from baseline (Figure 1). During the same period, patients with an annual PDMP review note in their medical record also increased from 4.1% to 19.6%, a 324% increase from baseline (Figure 2). Although the study period began in FY 2012 third quarter, FY 2014 first quarter was the baseline for PDMP review note data collection because VA providers were not legally allowed to access the SCRIPTS database prior to FY 2014.
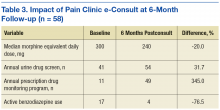
Impact of Interventions on High-Risk Opioid Prescribing
Patients who received an opioid prescription and a BZD derivative in the same fiscal quarter decreased 41.7% during the study period (Figure 3). A significant improvement was observed in each clinical variable at 6 months postintervention among high-dose COT patients who received an opioid safety review e-consult (Table 3). The median opioid dose per patient decreased 20% from baseline, from 300 mg MEDD to 240 mg MEDD. The number of patients with an annual UDS increased 31.7% from 41 to 54 patients. The number of patients with an annual PDMP review also increased 345%, from 11 patients to 49 patients. Finally, the number of patients with an active BZD order decreased > 75% from 17 patients at baseline to 4 patients at 6-month follow-up.
In the FY 2014 third quarter, prior to activation of the opioid safety review e-consult tool, 100 patients received high-dose COT. Follow-up at the conclusion of fourth quarter FY 2015 revealed 64 such patients, which represented a 36% decrease from baseline.
Discussion
During the study period, the POC used a variety of interventions from 4 distinct categories. Overall, these interventions successfully increased measures of appropriate COT monitoring (ie, UDS and PDMP utilization) and management of high-risk COT. Substantial improvements also were seen in the subgroup of patients receiving high-dose COT following creation and use of the opioid safety review e-consult tool.
Other VHA opioid management improvement initiatives were successful at reducing high-dose opioid prescribing through interventions similar to those described in this study. However, these initiatives did not address opioid monitoring practices or opioid/BZD combination therapy.25,26 To the authors’ knowledge, no previous opioid management improvement initiatives have reported improvements in provider use of a state PDMP database.
There are a number of factors that also may have helped lead to the successful outcomes observed during the study period. First, the creation of an informatics tool allowed for sustained interventions over time. While targeted interventions and patient/provider education were certainly beneficial, the impact of these efforts wanes as time moves forward. Inevitably, a patient’s and a provider’s focus move to the next important issue, and new patients meet the criteria of the original targeted intervention.
Group Health Cooperative implemented an opioid risk reduction initiative that successfully increased UDS use over a 2-year postimplementation period.21,26 While this initiative used a number of similar interventions to those implemented in this study (patient and provider education, targeted patient intervention), an informatics tool was not used. The annual UDS rate at the conclusion of the Group Health initiative was 50%, which contrasts with a final rate of 75.5% in this study. Although it is difficult to draw comparisons between the studies given differences in populations studied, periods of evaluation, and varying baseline annual UDS rates, the current study results demonstrate the potential effectiveness of informatics tools to help drive enduring changes in practice.
An additional factor that had a positive impact on outcomes the continued support and advocacy from RHJVAMC clinical and administrative leadership. A targeted review of all patients receiving concomitant BZDs and opioids would not be possible without mental health department leaders who believed in the value of the time consuming undertaking. Furthermore, an e-consult tool is effective only if actually submitted for patients and if a specialist’s recommendations are then followed by a PCP.
Finally, the interdisciplinary nature of the POC contributed to the success of each intervention described in this study. Patients receiving COT often have many complex physical, psychological, and social issues that must be considered in order to make a positive impact on patient care. To appropriately and effectively address these issues requires close collaboration between specialists from multiple disciplines.
Limitations
This study has several important limitations. First, its retrospective nature presents obvious documentation challenges. A second limitation is the brief period of evaluation following a number of POC interventions. For instance, 3 interventions took place in January 2015, leaving only 3 FY quarters of effectiveness data. Furthermore, increased awareness of the risks associated with opioid therapy in the VHA and the health care industry across the study period may have independently impacted the improvements observed in this study.