Malnutrition as a Fall Risk Factor
Eligibility Criteria and Baseline Characteristics
Chart reviews of veterans aged > 18 years experiencing a fall while hospitalized at the LSCVAMC between October 1, 2010 and October 31, 2012, were eligible to be included in this study. Each veteran needed to have 1 documented weight in a maximum of 24 months before the first fall and a minimum of 1 documented Hgb value prior to the first fall.
Patients were excluded if they had experienced a cerebrovascular accident or transient ischemic attack; a documented orthopedic fracture in the 12 months before the first fall; a documented amputation of a lower limb in the past 24 months; diagnosis of blindness; a lack of outpatient weight for greater than 24 months before the first fall; a history of volume overload, renal, cardiovascular, or other in nature during hospitalization; and alcoholism. Additionally, if any of the study investigators felt as though a patient had commorientes that made weight history inaccurate, those patients were excluded. Data were reviewed on 170 randomly selected subjects. A total of 50 subjects were excluded for not meeting the inclusion criteria; 120 individuals met eligible criteria. The patients who had experienced falls were divided into 2 groups: single-event fallers (1 fall documented during the study period) and recurrent fallers (2 or more falls documented during the study period). Fifty subjects were excluded from the final analysis because they met the following exclusion criteria: volume overload anytime in the 12 months before the documented fall (42); amputation of a lower limb before the fall (6); and prosthetic device alteration within the 12 months before the fall (3). One of the subjects was eliminated for both volume overload and amputation.
Data Collection
Data obtained from the Computerized Patient Record System review included age, gender, diagnosis, and body weight at the time of the first fall and 1 month, 3 months, 6 months, and 1 year before the first fall. Hemoglobin values at time of the first fall, 1 month, 3 months, 6 months, and 1 year before first documented fall also were collected. Vitamin D values and date of value also were collected. In year 2 of this multiphase retrospective review, charts again were reviewed and additional data collected, which included absence or presence of dementia along with type of dementia and the presence or absence of cancer. Year 2 data collection also included diagnosis of malnutrition by provider and registered dietitian assessment of degree of malnutrition.
Analysis
Data analysis comparing single-event fallers and frequent fallers was performed using IBM SPSS Statistic V22.0s. This pilot study has recognized weight loss and anemia as being associated with repeat falls. A 2-tailed t test was performed to evaluate differences in weight history, 25-hydroxyvitamin D, and Hgb characteristics between single fallers and frequent fallers. A repeated analysis of variance was performed to evaluate changes in weight and Hgb values over time for single and multiple falls. During phase 2 of this trial, a subanalysis comparing individuals with and without the diagnosis of dementia was conducted.
Results
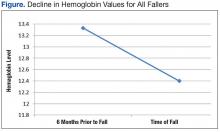
The average age of the patients was 68 years. There was a significant decline in Hgb levels in both single-event fallers and frequent fallers at 12 and 6 months before the first fall event (95% confidence interval; P = .001). One year before the first fall, 28% of eventual fallers met WHO criteria for the diagnosis of mild anemia. One year before the first fall, none of the eventual fallers met WHO criteria for moderate or severe anemia. Using the lab data just before the first fall, 10% of fallers met WHO criteria for mild anemia, 48% met WHO criteria for moderate anemia, and 31% met WHO criteria for severe anemia. The degree of anemia in single-event fallers when compared with multiple-event fallers was insignificant. Interestingly, the degree of decline of Hgb value during the 6 months before the first fall event was notable for all fallers (Figure).
Only 60 of the 120 included patients had a documented vitamin D level. At the time of the fall, 46 patients had moderate vitamin D deficiency, and 23 patients had severe vitamin D deficiency, defined as < 32 mg/dL. The authors speculate that vitamin D status declines with malnutrition and increases fall risk.
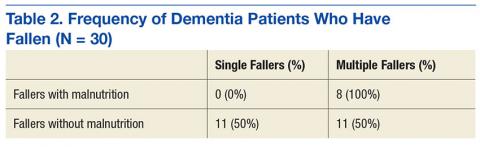
Thirty participants were included in the dementia arm; 36.7% were single-event fallers, and 63.3% were multiple-event fallers (Table 2). The average age of the groups was 76.7 years and 73.9 years, respectively. Physician diagnosis of malnutrition was collected for both single- and multiple-event fallers. Of the single-event fallers with dementia, none had a diagnosis of malnutrition before the first hospital fall; and of the multiple-event fallers with dementia, all had a diagnosis of malnutrition before their first hospital fall. Individuals with a diagnosis of dementia and malnutrition fall frequently (P = .0028).