Impact of a Drop-in Group Medical Appointment on Tobacco Quit Rates
One hundred thirty-six patients attended the DIGMA during the study period, but only 49 patients met the inclusion criteria. Patients also were excluded because they were not at the beginning of a quit attempt, were not receiving pharmacotherapy, or were not seen by an HCP to assess tobacco status after receiving tobacco cessation pharmacotherapy.
A total of 1,807 patients were identified as potential candidates for the PO group. Once the DIGMA patients were identified, an equal number of patients were randomly chosen for the PO group. To ensure that the PO group was random, the patient list was alphabetized, and patients were selected if they met the PO inclusion criteria, starting at the top of the list and moving down until the needed number was met.
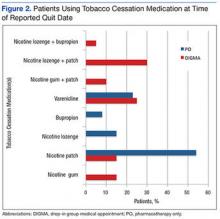
The primary endpoint was the tobacco quit rate within 1 year of starting pharmacotherapy for a new quit attempt. Tobacco use status was determined from the patient’s electronic medical record. A subgroup analysis was performed to determine the percentage of patients using each tobacco cessation medication or a combination of medications at the time of the reported quit date.
This study also looked at the number of DIGMA classes attended by patients who quit tobacco and the number of times patients switched pharmacotherapy during the 1-year time frame. A chi-square test was executed to evaluate the primary endpoint, and descriptive statistics were performed for the subgroup analysis. A P value of ≤ .05 was deemed significant.
Results
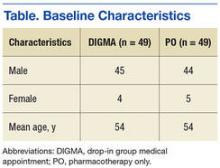
A total of 98 patients were included with 49 patients in each study arm. Baseline characteristics were similar between the groups with an average age of 54 years in both groups (Table). As shown in Figure 1, 40.8% of patients in the DIGMA group quit tobacco compared with 26.5% in the PO group (P = .19).
Discussion
The tobacco quit rate of veterans on pharmacotherapy who attended at least 1 DIGMA class was higher than the quit rate of veterans on pharmacotherapy only. Although the difference between quit rates was not statistically significant, the difference was clinically important. Every time a patient quits tobacco, years of negative health consequences and cost to the health care system may be prevented. Patients who quit tobacco and continue to attend DIGMA classes also can provide support and advice to others who are trying to quit.
The study results also suggest that the tobacco cessation DIGMA provided personalized care to veterans, as demonstrated by patients in the DIGMA group switching pharmacotherapy and using combination therapy more often. Access to pharmacists who can prescribe medications, change therapy, and assist with AEs gave patients the opportunity to determine the most efficacious therapy. Pharmacists also are aware of the pros and cons of the different tobacco cessation medications and are able to help patients pick the best medication to start with or change to.
Patients in the DIGMA group who quit tobacco attended an average of 1.4 classes. Those who attended the DIGMA may have been inherently more motivated to quit tobacco. However, the unique design of the DIGMA may have better equipped patients to quit tobacco after just 1 or 2 classes.
Limitations
Overall, an average attendance of 1.4 classes is a limitation; previous studies have shown that quit rates have a positive correlation with the number of counseling sessions attended.1 Another limitation is the small sample size. In addition, statistical power was not calculated. Tobacco use was not consistently documented in patients’ charts by the HCP and may not have been addressed at every visit. Some patients who quit tobacco may have been missed due to the lack of documentation of tobacco use status. Last, because reviewing a patient chart ended once documentation of tobacco cessation was found, some patients may have relapsed after quitting.
The study site likely could have offered better notice of the presence of the DIGMA. Although flyers and advertisements were available and posted, some tobacco-using patients may not have been aware of the DIGMA. The SFVAHCS could increase awareness of the program if the pharmacy provided a DIGMA flyer with each outpatient tobacco cessation prescription.
A larger, prospective study would be beneficial and might show statistically significant differences in tobacco quit rates. Further studies that address whether the DIGMA helps patients who have quit tobacco to remain tobacco free are needed.
Conclusion
Patients who attended the tobacco cessation DIGMA received personalized care and had a higher tobacco quit rate than did patients receiving standard treatment. However, due to study limitations, these results should be confirmed with future studies.
Acknowledgments
This material is the result of work supported with resources and the use of facilities at the Sioux Falls VA Health Care System in Sioux Falls, South Dakota.