Disease-Modifying Therapies in Multiple Sclerosis: Overview and Treatment Considerations
Compared with patients who have other chronic conditions, patients with MS experience diminished societal roles, along with decreased assessments in health, energy, and physical functions.25 These often lead to early exit from the workforce and limitations in household responsibilities, which further impact QOL.26 Including both direct and indirect costs of the disease, a patient with MS can expect a lifetime financial burden of nearly $1.2 million.27
Large population cohort studies in MS, along with MS registry studies of patients untreated with disease-modifying therapies, have shown reduced survival rates by an average of 7 to 14 years.23,28 Multiple sclerosis is the main cause of death in about 50% of cases (EDSS step 10), which is defined as “acute death due to brain stem involvement or to respiratory failure, or death consequent to the chronic bedridden state with terminal pneumonia, sepsis, uremia, or cardiorespiratory failure [and excluding] intercurrent causes of death.”23 For the remaining patients with MS, cause of death is similar to those of the general population, such as cardiovascular disease and cancer.23 However, the incidence of suicide is higher among patients with MS.23
All these factors underscore the importance of early diagnosis as well as early initiation of effective disease-modifying therapy.
Disease-Modifying Therapies
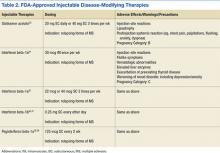
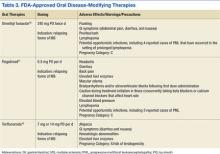
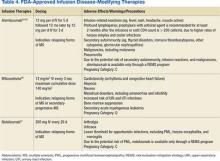
The goal of MS disease-modifying therapy is to reduce the early clinical and subclinical disease activity that eventually contributes to long-term disability.31,32 There are currently 13 FDA-approved disease-modifying therapies for MS. These include 7 self-injecting therapies, 3 oral therapies, and 3 infusion therapies. These 13 medications have 8 different mechanisms of action (MOA) that target distinct areas of the immune-mediated disease process. They also differ in their frequencies and routes of administration in addition to their adverse effect (AE) profiles (Tables 2, 3, and 4).
Treatment Considerations
In 1993, interferon beta-1b became the first FDA-approved MS medication. In the following 2 decades, there became 12 additional FDA-approved medications for MS, beginning with other injectables. The first infusion therapy was introduced in 2004, followed by various oral medications. The treatment landscape continues to change rapidly. This therapeutic revolution has occurred largely due to the improved understanding of the pathophysiology of MS and unquestionably has improved the prognosis and overall QOL for patients. The question is no longer how to treat MS but rather how to personalize and optimize treatment for each patient.20
Despite all available treatment options, none are curative, and none have been proven to offer neuroprotection or contribute to neural repair. To date, no studies have led to FDA-approved therapies for PPMS. Further, the efficacy of any of these medications varies from patient to patient. Due largely to the lack of biomarkers for disease activity and treatment response, drug efficacy continues to be measured according to the current gold standard, which is identification of gadolinium-enhancing lesions in the white matter on magnetic resonance imaging (MRI), combined with other markers of disease, including clinical relapse rate and confirmed disability progression.19 In general, the injectable therapies are expected to protect against about 20% to 35% of relapses; the oral agents, 50% to 55%; and the infusion therapies, > 60%.2
In conjunction with a medication’s efficacy rate and safety profile, the frequency and route of administration also must be considered. In general, MS medications are exceedingly expensive, some costing up to tens-of-thousands of dollars per year.48 All these factors have the real potential to negatively impact patient adherence. Nonadherence and gaps in treatment have been correlated with increased rates of relapses and progression of disability as well as negative MRI outcomes.49-53
When to Initiate Treatment
Once a patient is diagnosed, a common question is, when is the right time to initiate treatment? The primary target of the current MS medications is to decrease CNS inflammation (relapses). The ideal time to start treatment is as promptly as possible after confirmation of the diagnosis to combat the early inflammatory relapsing phase of the disease. There seems to be an early window in the disease course when achieving disease control can have a profound impact on long-term disability. Disease control is typically defined as decreasing relapses, slowing the accumulation of lesions visualized on MRI, and preventing the disability that occurs from both incomplete recovery after relapses and overall disease progression.54,55