The Social Worker’s Role in Delirium Care for Hospitalized Veterans
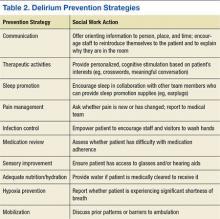
The goals of delirium treatment are to identify and reverse its underlying cause(s).29 Because delirium is typically multifactorial, an HCP must carefully consider the various sources that could have initiated a change in mental status. Delirium may be prevented if HCPs can reduce patient risk factors. The 2010 National Institute for Health and Clinical Excellence (NICE) Delirium Guideline recommended a set of prevention strategies to address delirium risk factors (Table 2).12
As a member of the health care team, social workers can help prevent delirium through attention to pain management, infection control, medication review, sensory improvement, adequate nutrition and hydration, hypoxia prevention, and mobilization.12No pharmacologic approach has been approved for the treatment of delirium.30 Drugs may manage symptoms associated with delirium, but they do not treat the disease and could be associated with toxicity in high-risk patients. However, there are a variety of nonpharmacologic preventative measures that have proven effective. Environmental interventions to prevent delirium include orientation, cognitive stimulation, and sensory aids. A 2013 meta-analysis of 19 delirium prevention programs found that most were effective in preventing delirium in patients at risk during hospitalization.31 This review found that the most successful programs included multidisciplinary teams providing staff education and therapeutic cognitive activities.31 Social workers can encourage and directly provide such services. The Delirium Toolbox is a delirium risk modification program that was piloted with frontline staff, including social workers, at the VA Boston Healthcare System in West Roxbury, Massachusetts, and has been associated with restraint reduction, shortened length of stay (LOS), and lower variable direct costs.32
Social Worker Role
Several studies, both national and international, have indicated that little has been done over the past 2 decades to increase the diagnosis of delirium, because only 12% to 35% of delirium cases are clinically detected within the emergency department and in acute care settings.33-37 Patients may hesitate to report their experience due to a sense of embarrassment or because of an inability to describe it.38
Social workers are skilled at helping individuals feel more at ease when disclosing distressing experiences. Delirium is relevant to HCPs and hospital social workers with care transition responsibilities, because delirium detection should impact discharge planning.1,39 Delirium education needs to be included in efforts to improve transitions from intensive care settings to lower levels of care and from lower levels of care to discharge.40 Hospital social workers are in a position to offer additional support because they see patients at a critical juncture in their care and can take steps to improve postdischarge outcomes.41
Prior to Onset
Social workers can play an important role prior to delirium onset.42 Patient education on delirium needs to be provided during the routine hospital intake assessment. Informing patients in advance that delirium is common, based on their risk factors, as well as what to expect if delirium is experienced has been found to provide comfort.38 Families who anticipated possible delirium-related confusion reported that they experienced less distress.38
Related: Baseball Reminiscence Therapy for Cognitively Impaired Veterans
During hospitalization, social workers can ascertain from families whether an alteration in mental status is a rapid change, possibly indicating delirium, or a gradual dementia onset. The social work skills of advocacy and education can be used to support delirium-risk identification to avoid adverse outcomes.43 When no family caregiver is present to provide a history of the individual’s cognitive function prior to hospitalization, the social worker may be the first to notice an acute change in cognitive status and can report this to the medical team.
During Delirium
Lack of patient responsiveness and difficulty following a conversation are possible signs of delirium. This situation should be reported to the medical team for further delirium assessment and diagnosis.4 The social worker can also attempt to determine whether a patient’s presentation is unusual by contacting the family. Social work training recognizes the important role of the family.44 Social workers often interact with families at the critical period between acute onset of delirium in the hospital and discharge.42 Studies have shown that delirium causes stress for the patient’s loved ones. Moreover, caregivers of patients who experience the syndrome are at a 12 times increased risk of meeting the criteria for generalized anxiety disorder.30 In one study, delirium was rated as more distressing for the caregivers who witnessed it than for the patients who experienced it.38 Education has been shown to reduce delirium-related distress.30
In cases where delirium is irreversible, such as during the active dying process, social workers can serve in a palliative role to ease family confusion and provide comfort.30 The presence of family and other familiar people are considered part of the nonpharmacologic management of delirium.28