Step-by-step evaluation and treatment of shoulder dislocation
Tailor management decisions by taking into account the patient’s age, the direction of instability, functional demands, risk of recurrence, and associated injuries.
PRACTICE RECOMMENDATIONS
› Refer first-time dislocation in patients younger than 20 years or who have a displaced fracture to an orthopedic surgeon. A
› Order magnetic resonance imaging (MRI) for all patients with a suspected rotator cuff tear. A
› Send patients with weakness of the rotator cuff—but no tear on MRI—for evaluation by electromyography and nerve-conduction studies. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Combined, apprehension and relocation tests to identify anterior shoulder instability have been shown to significantly improve specificity while maintaining sensitivity.8
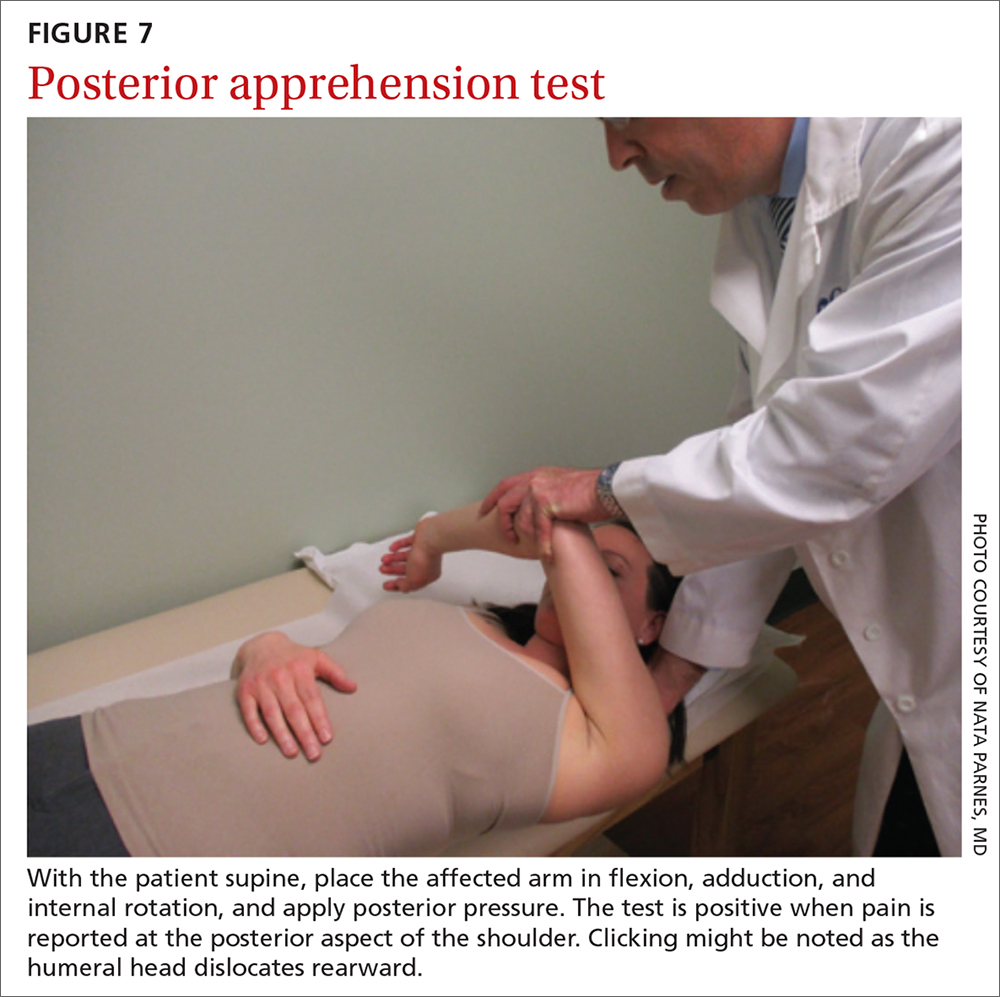
The posterior apprehension test is used to assess posterior instability. The patient is supine; the affected arm is placed in flexion, adduction, and internal rotation; and posterior pressure is applied (FIGURE 7). A positive test is noted when pain is reported at the posterior aspect of the shoulder. Clicking might be noted as the humeral head dislocates rearward.1
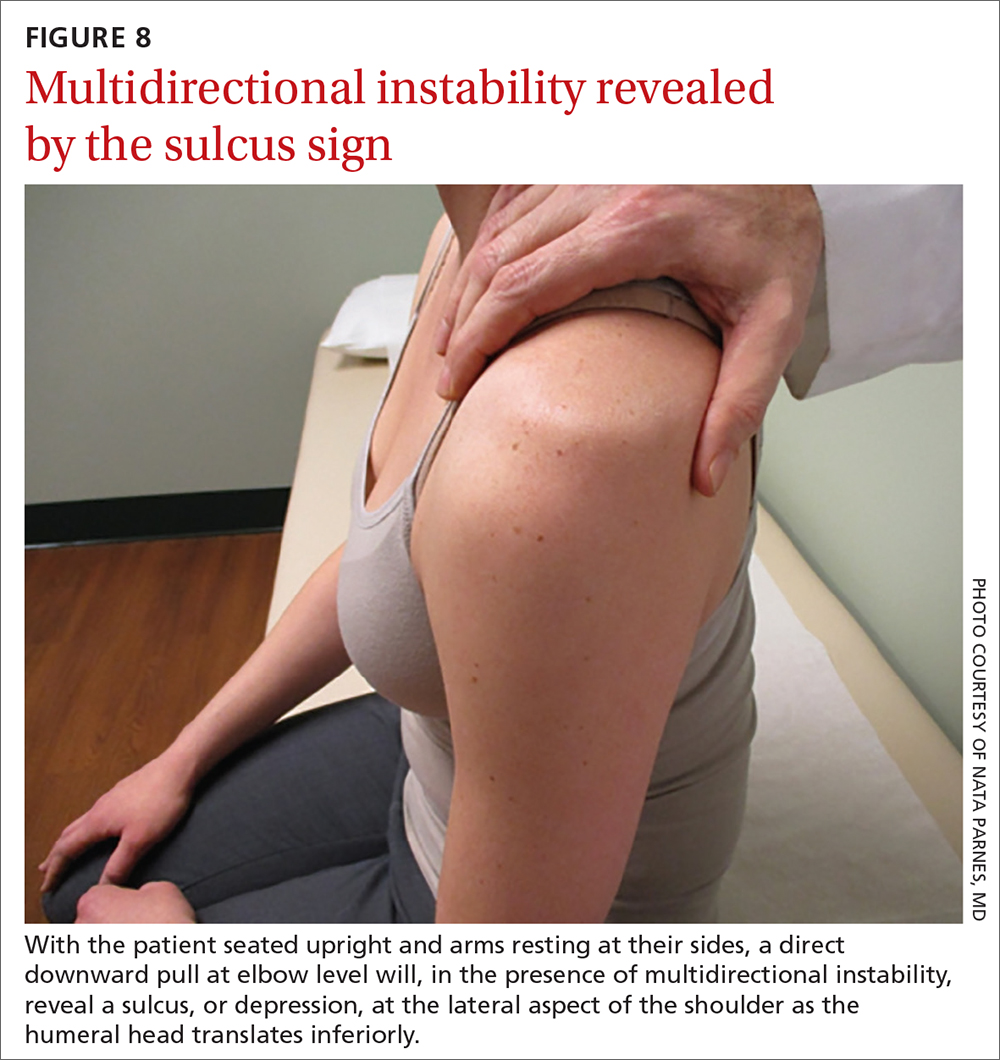
Sulcus sign. Multidirectional instability is elicited using the sulcus sign. While the patient is seated upright, arms resting at their sides, a direct downward pull at elbow level will, when positive, reveal a depression (sulcus) at the lateral aspect of the affected shoulder as the humeral head translates inferiorly (FIGURE 8). A positive sulcus sign is documented in 3 grades, according to the amount of translation1:
- Grade I: < 1 cm
- Grade II: 1-2 cm
- Grade III: > 2 cm.
Neurovascular status should be verified at every physical evaluation, with motor and sensory function tested in the axillary, musculocutaneous, median, radial, and ulnar nerve distributions. If nerve injury is suspected, electromyography and nerve-conduction testing is indicated.9-13 Vascular compromise is much less common but equally important to assess.11
Use of imaging
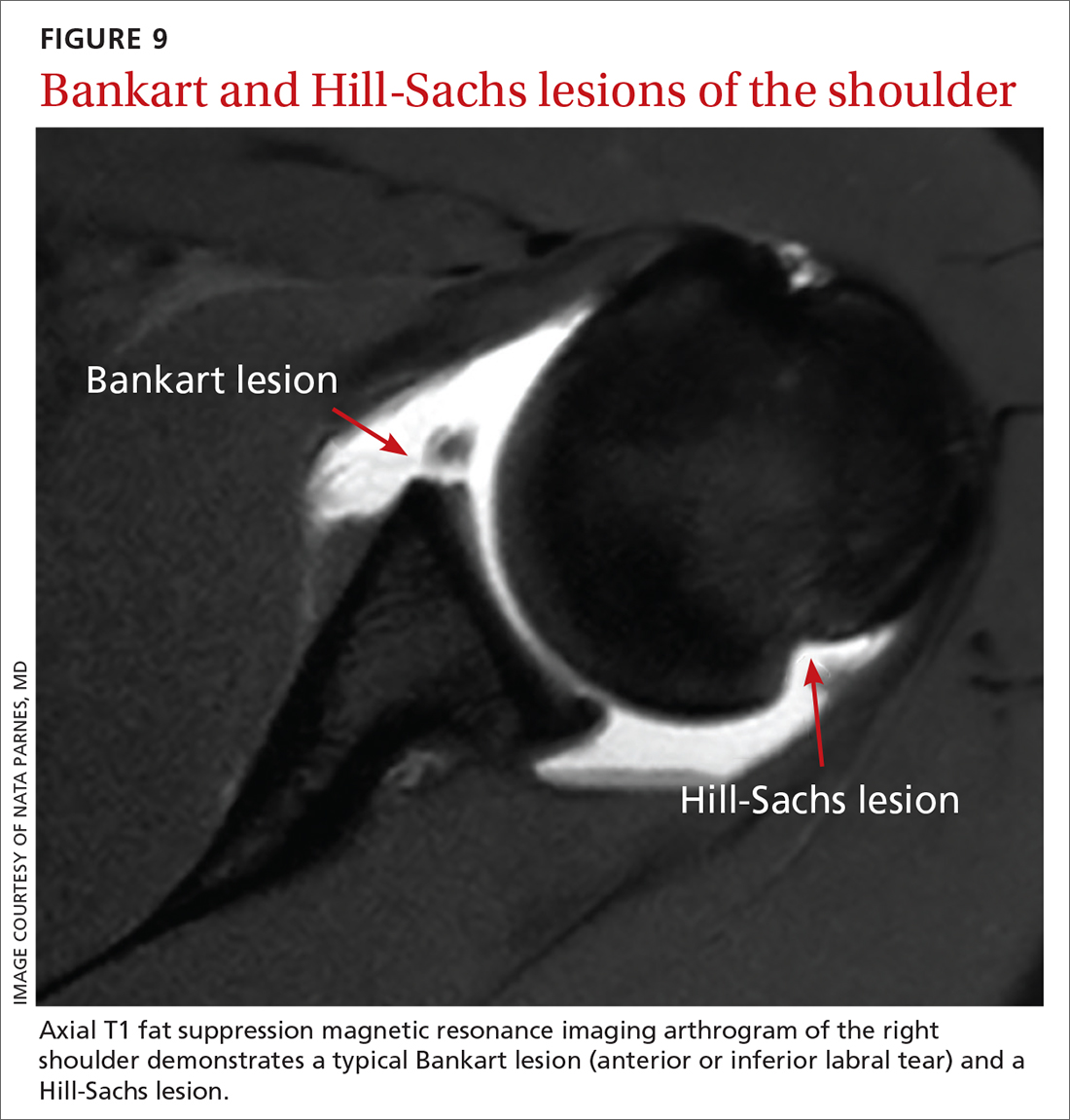
Post-reduction radiographs, including internal and external AP—and especially axillary—views are invaluable. Not only do they help to ensure reduction, but they also help to assess for fracture. A magnetic resonance imaging (MRI) arthrogram is the preferred imaging modality if a labral tear is suspected (FIGURE 9). Other concomitant shoulder injuries, such as subtle bone fracture, rotator cuff tear, and biceps pathology can also be reliably diagnosed with noncontrast MRI.
Continue to: Roadmap for treatment






