Step-by-step evaluation and treatment of shoulder dislocation
Tailor management decisions by taking into account the patient’s age, the direction of instability, functional demands, risk of recurrence, and associated injuries.
PRACTICE RECOMMENDATIONS
› Refer first-time dislocation in patients younger than 20 years or who have a displaced fracture to an orthopedic surgeon. A
› Order magnetic resonance imaging (MRI) for all patients with a suspected rotator cuff tear. A
› Send patients with weakness of the rotator cuff—but no tear on MRI—for evaluation by electromyography and nerve-conduction studies. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Follow-up actions. Before discharging the patient after reduction of a dislocation, it is essential to:
- perform post-reduction evaluation of shoulder stability at different levels of abduction
- perform a thorough neurovascular assessment
- obtain an anteroposterior (AP) radiograph to ensure proper positioning of the glenohumeral joint.
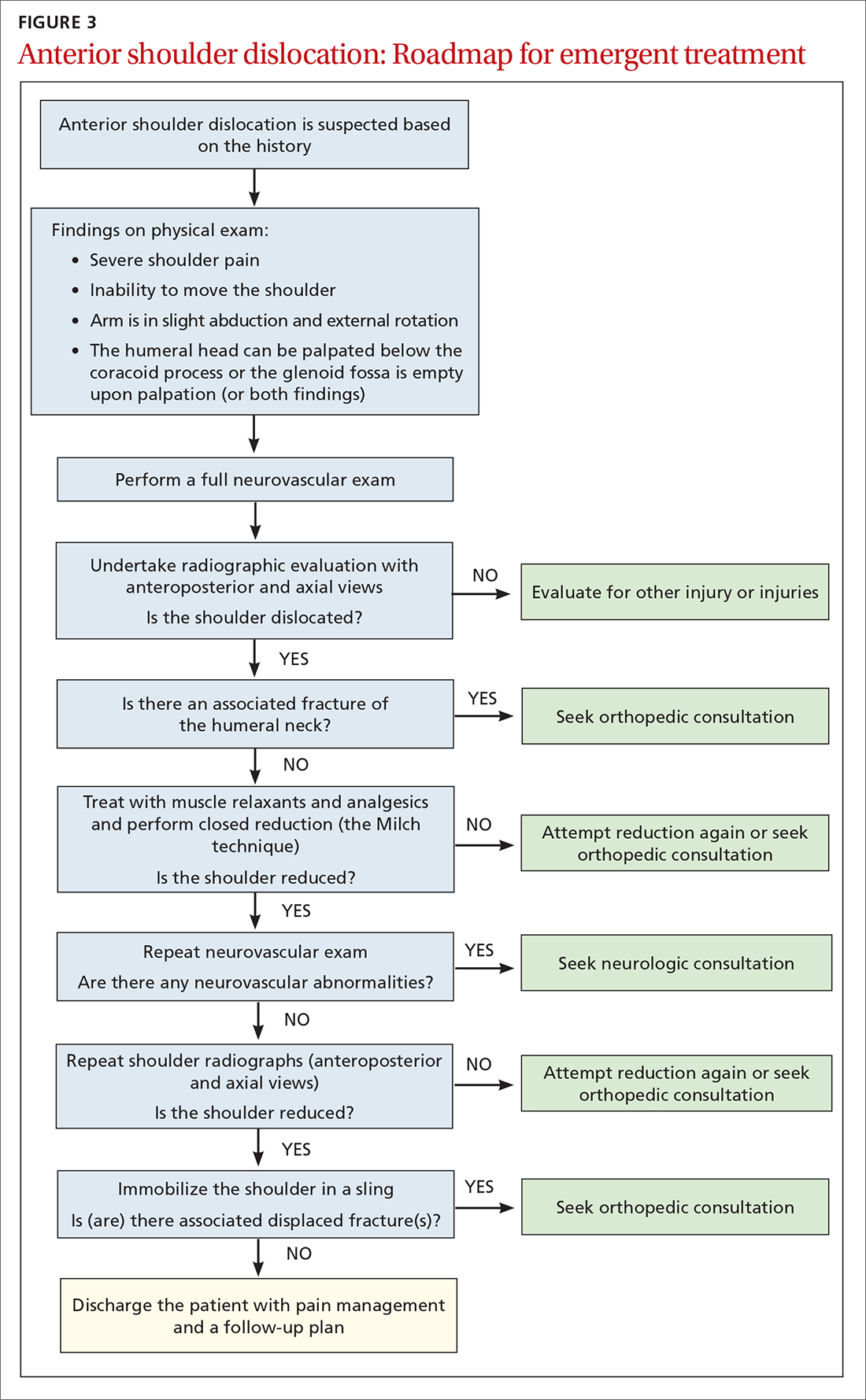
The reduced shoulder should be immobilized in a sling. The discharge plan should include pain management for several days and a follow-up appointment in 5 to 8 days with the primary care provider2 (FIGURE 3).
Follow-up evaluation by the primary care provider
History. Prior to the initial examination at follow-up, obtain a comprehensive history that includes the nature of the injury and the direction of force that was placed on the shoulder. Determine whether the shoulder was reduced spontaneously or required manual reduction in the field or an emergency department. Note any associated injury sustained concurrently and the presence (or absence) of neck pain, numbness, tingling, or weakness in the affected arm.
Physical exam starts with thorough inspection of the affected shoulder, with comparison to the contralateral side, at rest and during shoulder motion. Palpation to reveal points of tenderness should include the anterior joint line, acromioclavicular joint, bicipital groove, subacromial space, acromion, and greater tuberosity.
Following inspection and palpation, assess active and passive range of motion in forward elevation, abduction, internal and external rotation at the side of the body, and internal and external rotation in shoulder abduction. Assessment might be limited by pain and apprehension, and should be performed within the patient’s comfortable range of motion.
Continue to: Once range of motion...






