Step-by-step evaluation and treatment of shoulder dislocation
Tailor management decisions by taking into account the patient’s age, the direction of instability, functional demands, risk of recurrence, and associated injuries.
PRACTICE RECOMMENDATIONS
› Refer first-time dislocation in patients younger than 20 years or who have a displaced fracture to an orthopedic surgeon. A
› Order magnetic resonance imaging (MRI) for all patients with a suspected rotator cuff tear. A
› Send patients with weakness of the rotator cuff—but no tear on MRI—for evaluation by electromyography and nerve-conduction studies. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Multidirectional instability is more frequently attributable to congenital hyperlaxity of the glenohumeral joint capsule, rather than to acute injury. However, athletes can also develop capsular laxity from repetitive microtrauma to the shoulder.5
Emergent reduction: Prompt action needed
Acute dislocation of the shoulder should be reduced as soon as possible to minimize neurovascular injury and patient discomfort. (Typically, but not always, this is done in the emergency department.) It is crucial to have effective muscle relaxation before any attempt at reduction, to minimize the risk of iatrogenic injury to bone, cartilage, tendons, and neurovascular structures.
Muscle relaxation can be facilitated with intravenous midazolam or other agents, as specified by institutional protocol. Intra-articular lidocaine injection or intravenous fentanyl is often utilized in conjunction with the sedating agent to reduce pain and further accommodate relaxation.
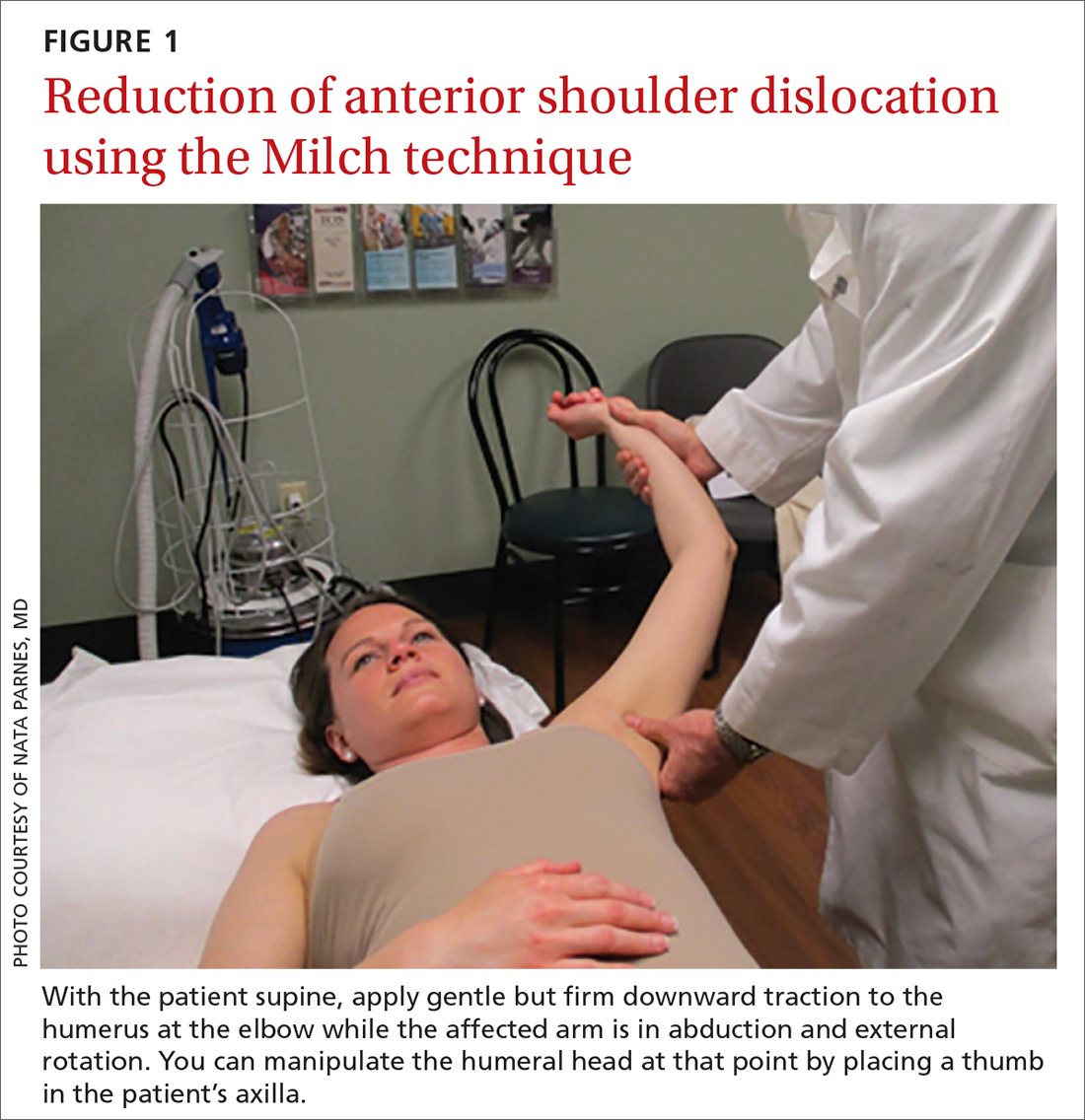
Anterior reduction. Any one of several techniques can be used to perform emergent reduction of anterior shoulder dislocations, all of which have demonstrated success. The Milch technique is among the least traumatic for effective reduction.6 In this technique (FIGURE 1), the patient is supine; gentle but firm downward traction is applied to the humerus at the elbow of the affected arm while the arm is in abduction and external rotation. The provider can manipulate the humeral head at that point by placing a thumb in the patient’s axilla; the arm can also be further internally rotated and adducted until reduction is achieved.
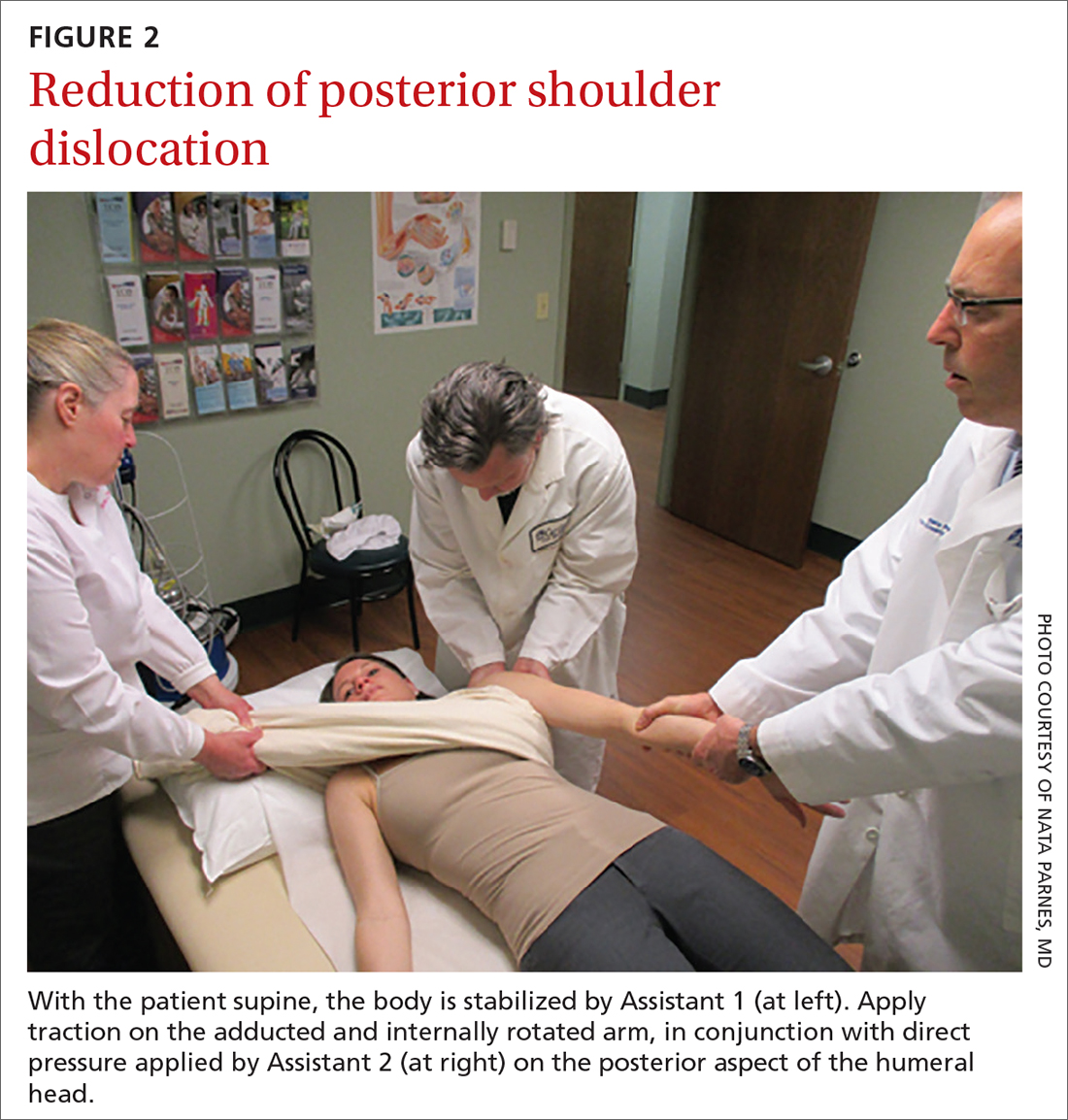
Posterior reduction of a dislocation is performed while the patient is supine, with the body stabilized. Traction is applied on the adducted and internally rotated arm in conjunction with direct pressure on the posterior aspect of the humeral head (FIGURE 2).
Continue to: Follow-up actions






